Cancer precursor project - characteristics of premalignant precursors, part 1 (carcinomas)
3 April 2024, revised 17 May 2024
The goal of our cancer precursor project is to better understand how cancer arises by compiling a regularly updated spreadsheet of all distinct human cancers (now 1230) and their premalignant precursors (now 185).
Although premalignant precursors have been identified for 15.0% of distinct malignancies, the percentage varies widely by pathology subspecialty:
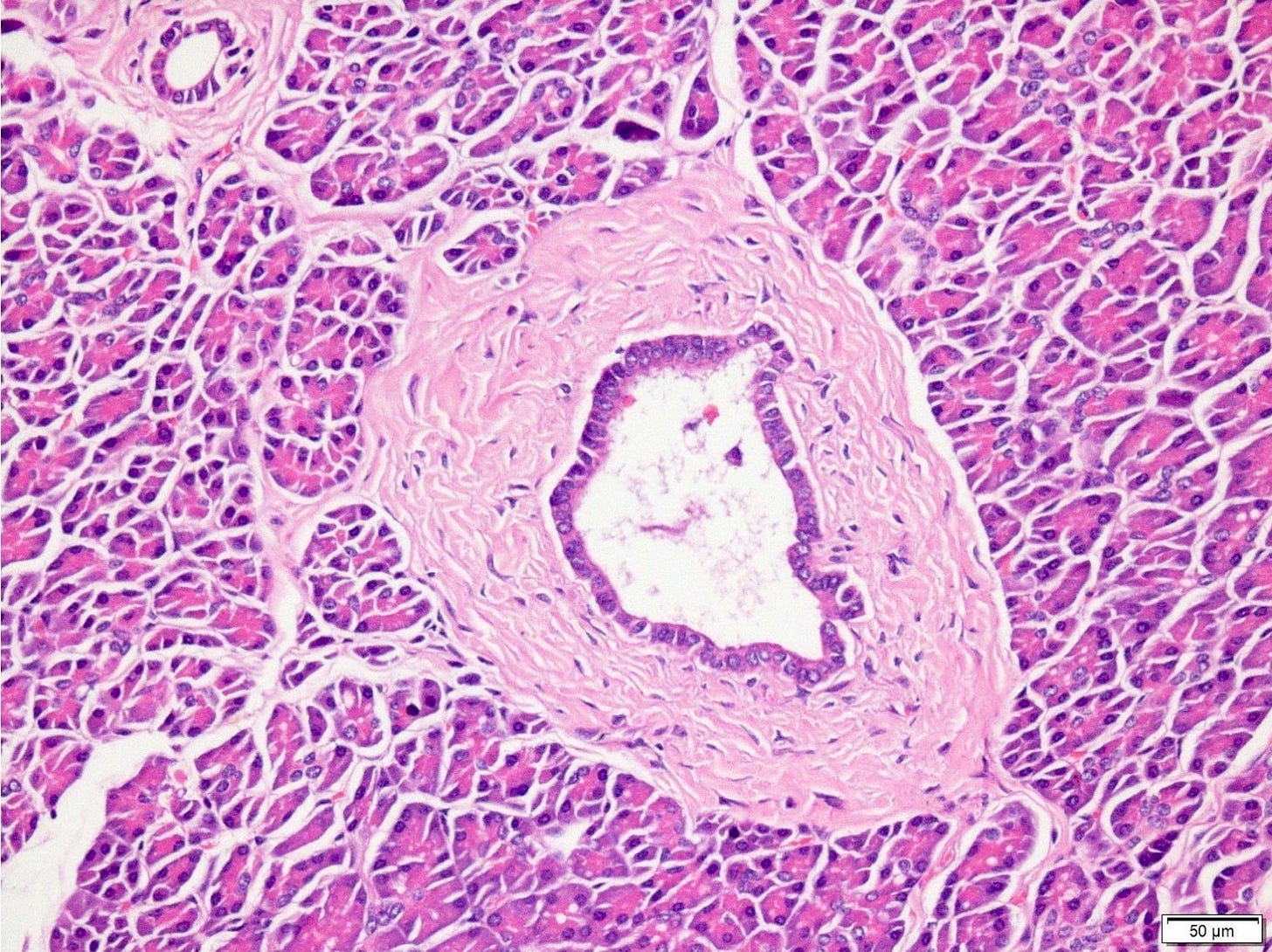
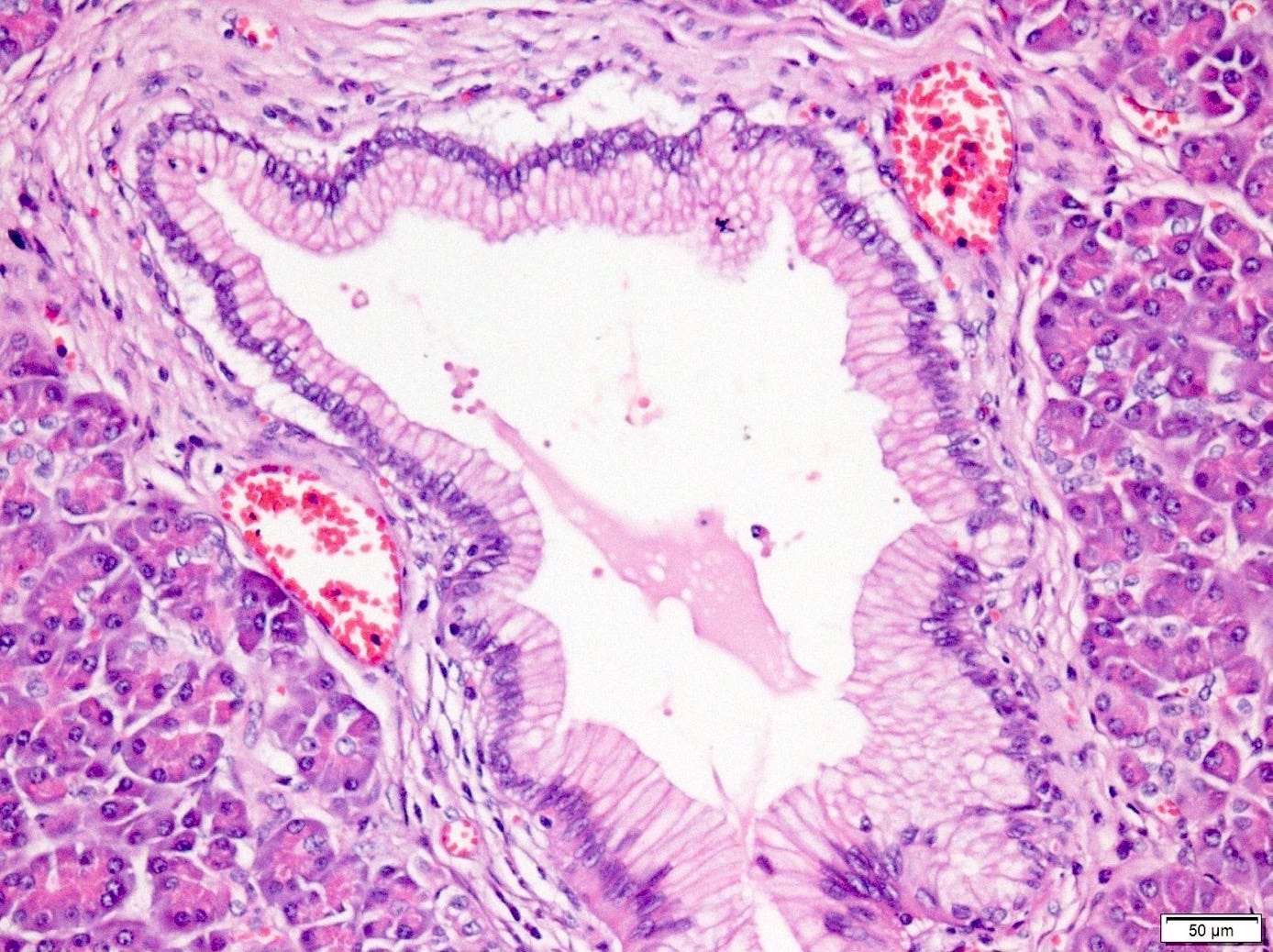
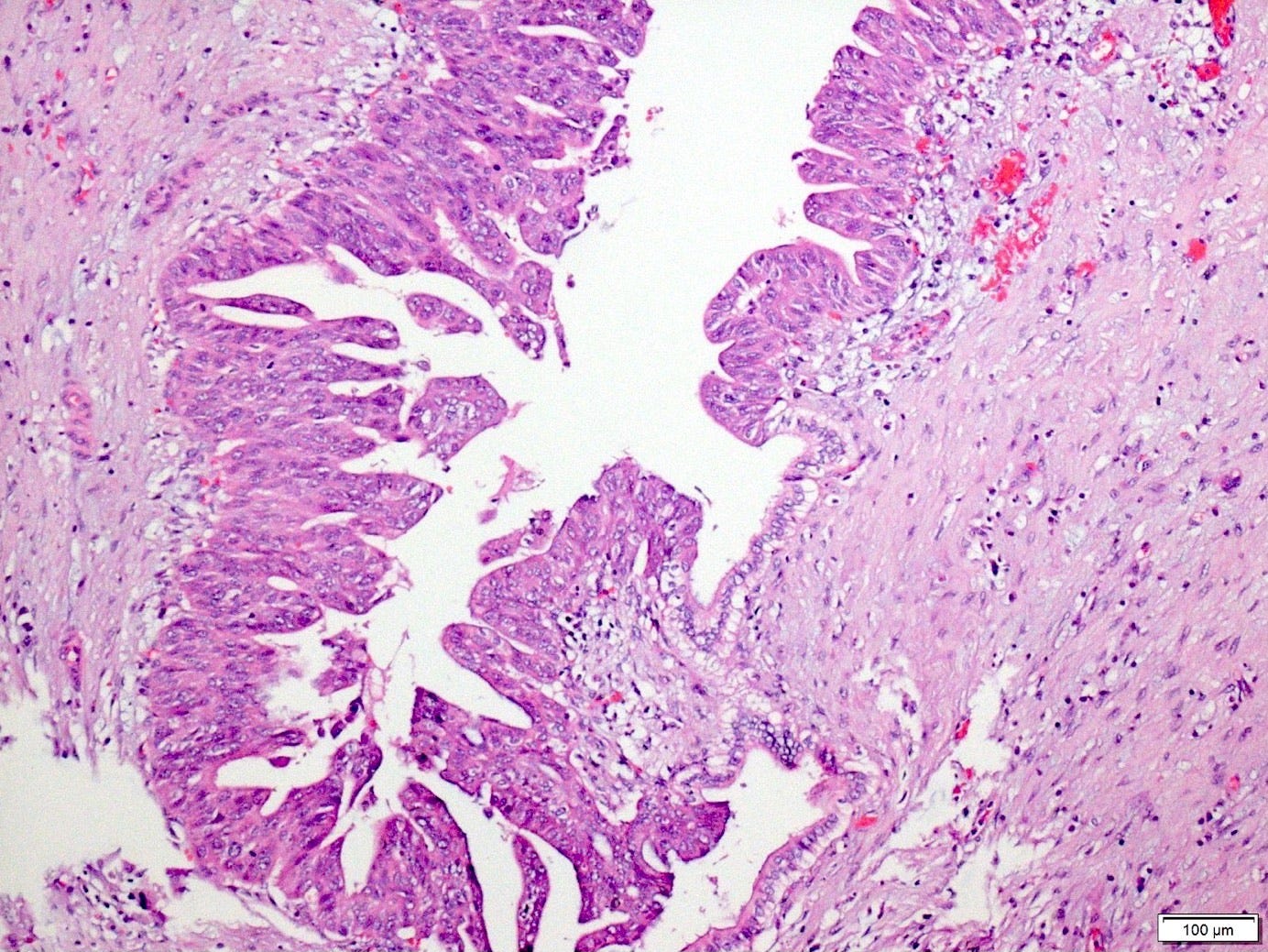
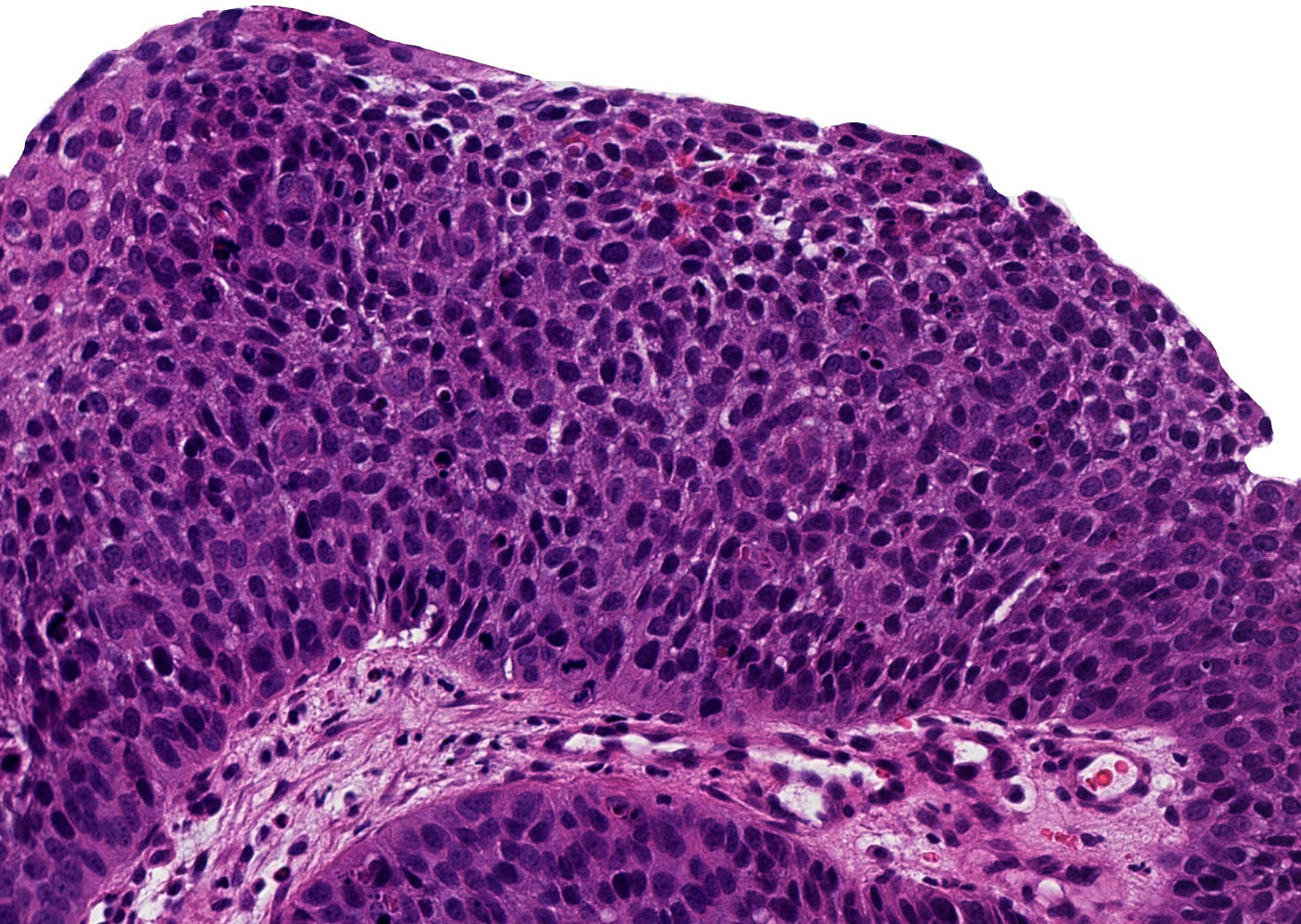
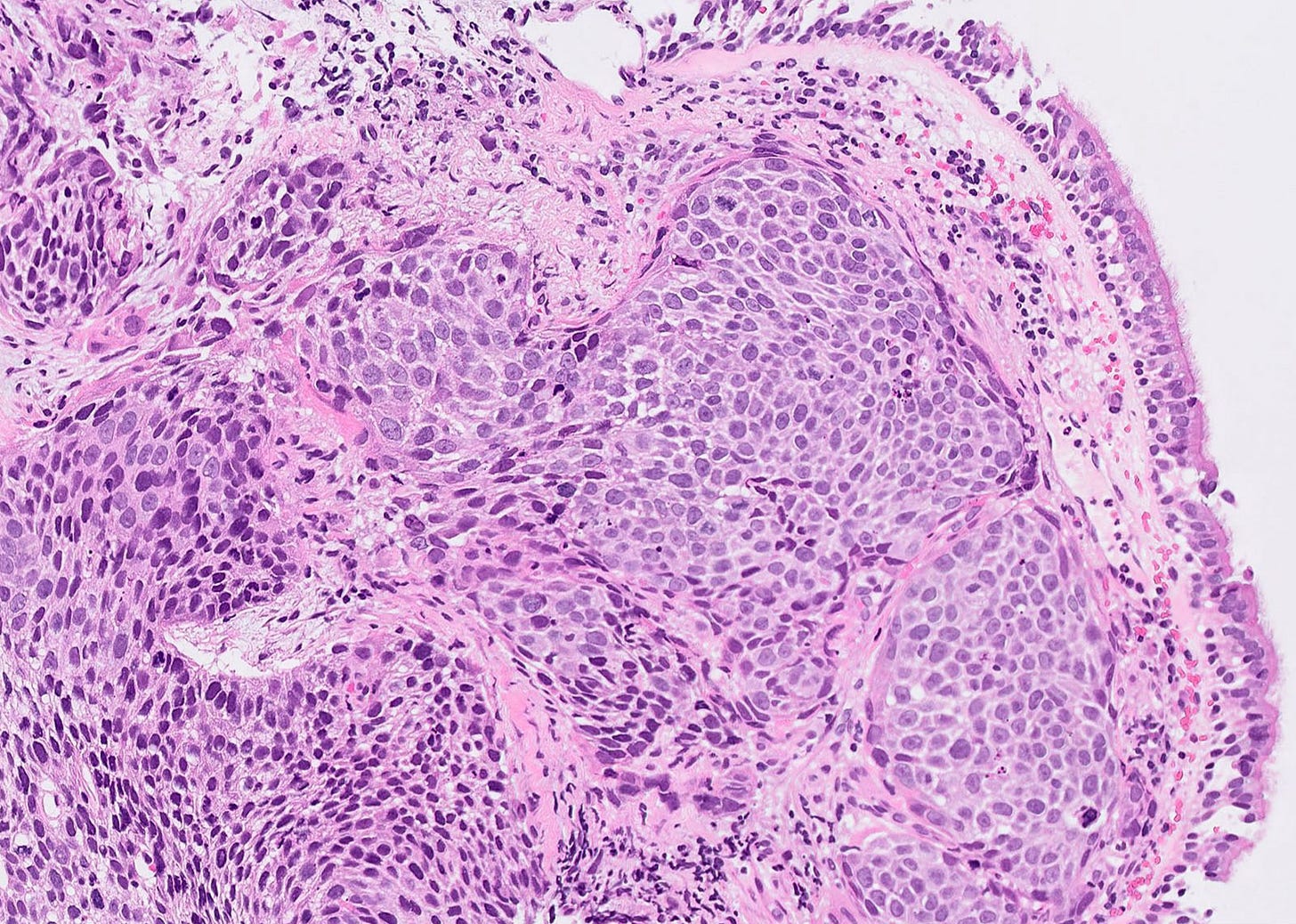
The premalignant precursors of carcinomas (invasive epithelial cancers) have been characterized based on the intraepithelial neoplasia model, which describes epithelial lesions that are premalignant, microscopic and noninvasive (particularly high grade lesions) that can progress to carcinomas. Classification is based on the highest degree of cytologic atypia identified. Some of these premalignant lesions are termed dysplasia (low grade or high grade) or carcinoma in situ. Carcinomas may also arise from metaplastic lesions (metaplasia: the reversible substitution of one type of fully differentiated cell for another within a given tissue, such as Barrett esophagus). Examples of the intraepithelial neoplasia or dysplastic pathways follow for pancreatic adenocarcinoma and lung squamous cell carcinoma:
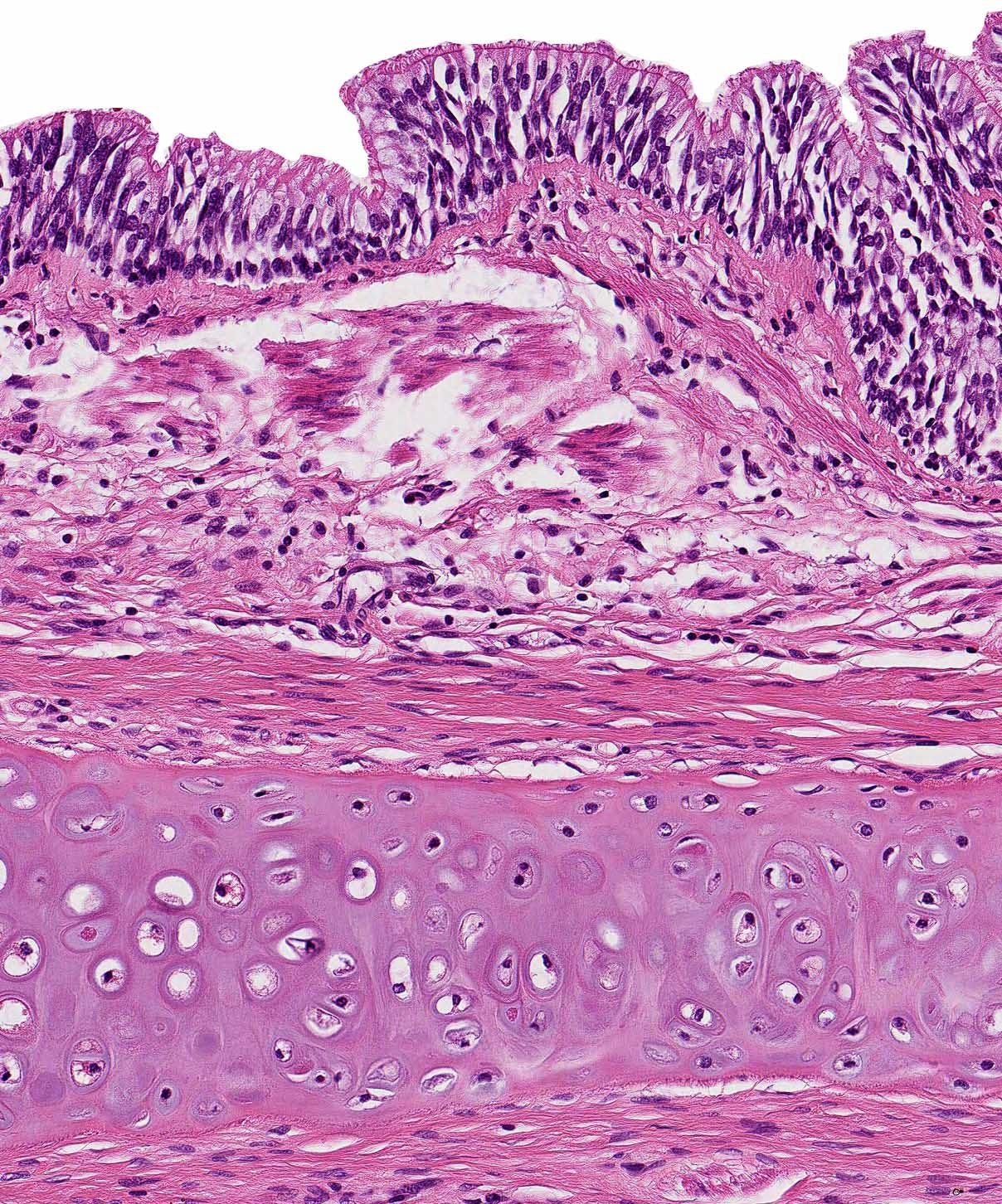
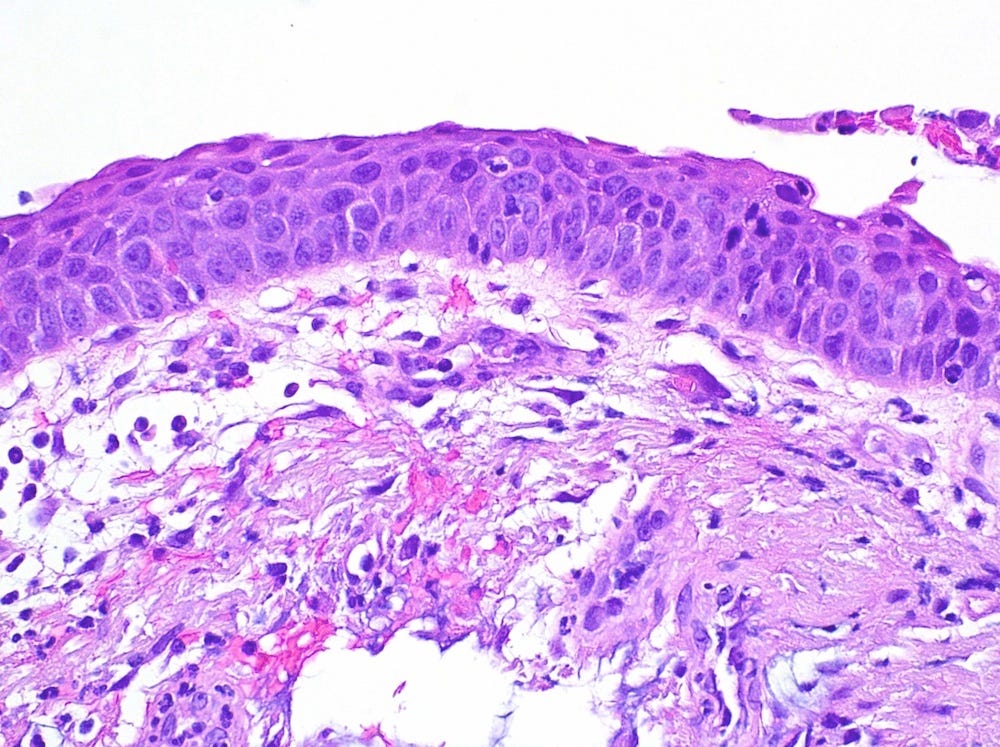
Malignant pathway of pancreatic adenocarcinoma
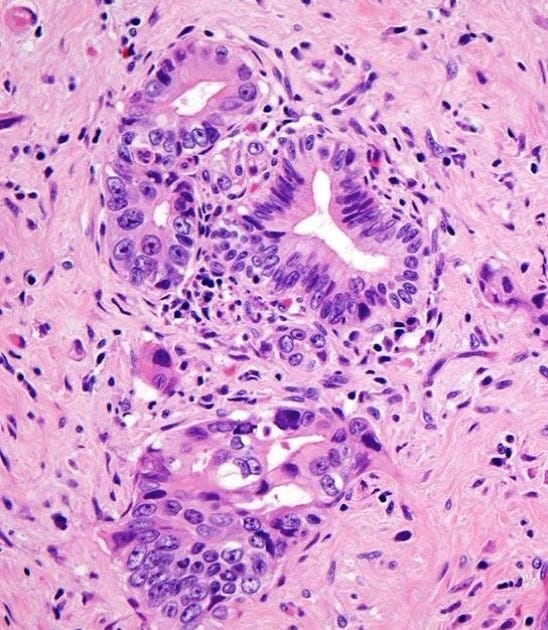
Malignant pathway of pulmonary squamous cell carcinoma
Premalignant precursors, although uncommon for some pathology subspecialties (neuropathology, dermatopathology, bone & soft tissue pathology and hematopathology), are common at epithelial sites - representative premalignant precursors are listed below:
Breast:
Ductal carcinoma in situ, atypical ductal hyperplasia
GI / liver:
Anus: anal intraepithelial neoplasia (anal IEN / AIN), Buschke-Löwenstein tumor
Appendix: low grade and high grade appendiceal mucinous neoplasm (LAMN / HAMN), tubular adenoma
Colon: conventional adenoma, serrated lesions, dysplasia associated with inflammatory bowel disease
Esophagus: Barrett related dysplasia, esophageal squamous intraepithelial neoplasia / squamous dysplasia
Gallbladder & extrahepatic bile ducts: intracholecystic papillary neoplasm, biliary intraepithelial neoplasia / adenoma (BilIN)
Liver & intrahepatic bile ducts: hepatic intraductal papillary neoplasm of the bile ducts
Pancreas: pancreatic intraepithelial neoplasia (PanIN), intraductal papillary mucinous neoplasm (IPMN)
Small intestine & ampulla: intra-ampullary papillary tubular neoplasm
Stomach: dysplasia
GU / adrenal gland:
Bladder & urothelial tract: dysplasia, carcinoma in situ
Penis & scrotum: penile intraepithelial neoplasia (PeIN)
Prostate gland & seminal vesicles: prostatic intraepithelial neoplasia (HGPIN)
No premalignant epithelial precursors were identified in the adrenal gland, kidney and testis.
Gynecologic:
Cervix: squamous intraepithelial lesion (high grade /HSIL), low grade / LSIL, adenocarcinoma in situ (AIS)
Fallopian tubes & broad ligament: serous tubal intraepithelial carcinoma (STIC)
Ovary: serous borderline tumor, mucinous borderline tumor
Uterus: endometrial atypical hyperplasia / endometrioid intraepithelial neoplasia (AH / EIN)
Vulva & vagina: vaginal intraepithelial neoplasia (VAIN), vulvar intraepithelial neoplasia (VIN)
No premalignant epithelial precursors were identified in the placenta and peritoneum.
Head & neck:
Ear: external ear-squamous dysplasia
Eye: conjunctival intraepithelial neoplasia
Larynx, hypopharyx & trachea: dysplasia
Mandible & maxilla: ameloblastoma, calcifying epithelial odontogenic tumor
Nasal cavity & nasopharynx: squamous dysplasia, sinonasal papilloma with dysplasia, intestinal metaplasia
Oral cavity & oropharynx: epithelial dysplasia
Salivary glands: adenocarcinoma in situ, pleomorphic adenoma
No premalignant epithelial precursors were identified in the thyroid & parathyroid glands.
Thoracic:
Lung: atypical adenomatous hyperplasia, adenocarcinoma in situ, squamous cell carcinoma in situ
No premalignant epithelial precursors were identified in the heart, mediastinum and pleura.
We believe that studying these precursor lesions will help identify precursor lesions that we believe exist but are currently unknown, such as in the CNS (central nervous system or brain) and soft tissue.
Part 2 will discuss subspecialties with fewer identified precursors.
If you like these essays, please share them with others.
Click here for the Index to Nat’s blog on Cancer and Medicine
Follow us on Substack, LinkedIn, Threads and Instagram (npernickmich) and Tribel (@nat385440b).essays
Follow our Curing Cancer Network through our Curing Cancer Newsletter, on LinkedIn or Twitter or the CCN section of our PathologyOutlines.com blog. Each week we post interesting cancer related images of malignancies with diagnoses plus articles of interest. Please also read our CCN essays.
Latest versions of our cancer related documents:
American Code Against Cancer (how you can prevent cancer)
Email me at Nat@PathologyOutlines.com - Unfortunately, I cannot provide medical advice.
I also publish Notes at https://substack.com/note. Subscribers will automatically see my notes.




