Cancer precursor project - characteristics of premalignant precursors, part 2 (neuropathology-brain and eye tumors)
24 April 2024, revised 17 May 2024
The goal of our cancer precursor project is to better understand how cancer arises by compiling a regularly updated spreadsheet of all distinct human cancers (currently 1,230) and their premalignant precursors (currently 185). Note: these numbers change based on our research and feedback from pathologists and scientists worldwide.
In part 1 of this series, we noted that the percentage of identified precursors varies widely by pathology subspecialty (see table below) and discussed precursors for subspecialties with epithelial sites (breast, head & neck, gyn, GI / liver, GU / adrenal and thoracic). In this essay, we discuss actual and possible malignant precursors associated with neuropathology.
In neuropathology, no precursor has been identified for any of the 100 CNS malignancies listed. How is this possible? It seems unlikely that pathologists and other scientists have overlooked them. Perhaps the traditional concept of precursor does not apply:
Cancer precursors are the tissue antecedents of cancer. They are distinguished from biomarkers in that they reflect a morphologic as opposed to a merely biochemical or genetic association with a specific cancer. Precursors to cancers are increasingly recognized as universal, relevant to carcinogenesis, and providing a unique potential for primary and secondary prevention. As the molecular, imaging, and genomic tools to investigate them evolve, it is becoming increasingly evident that virtually all malignancies are preceded by these clinically silent states where the molecular lesions that characterize the specific cancer emerge. Caporaso 2013 [emphasis added]
However, based on our work, it now appears that most CNS malignancies do NOT have a morphologic precursor. A CNS malignancy may be initiated by a defining mutation in a single stem or progenitor cell or small cluster of cells that multiplies and acquires additional malignant properties over time. Due to its small size, detection may not be possible, at least with current methods, until it is large enough to be clinically evident.
For glioblastoma, the most common brain malignancy in adults, we recently speculated that its premalignant precursor might consist of “milder” versions of its defining molecular or histologic changes in a nonmalignant context, although we now believe, based on further reflection, that there may be no detectable precursor to this and other CNS tumors.
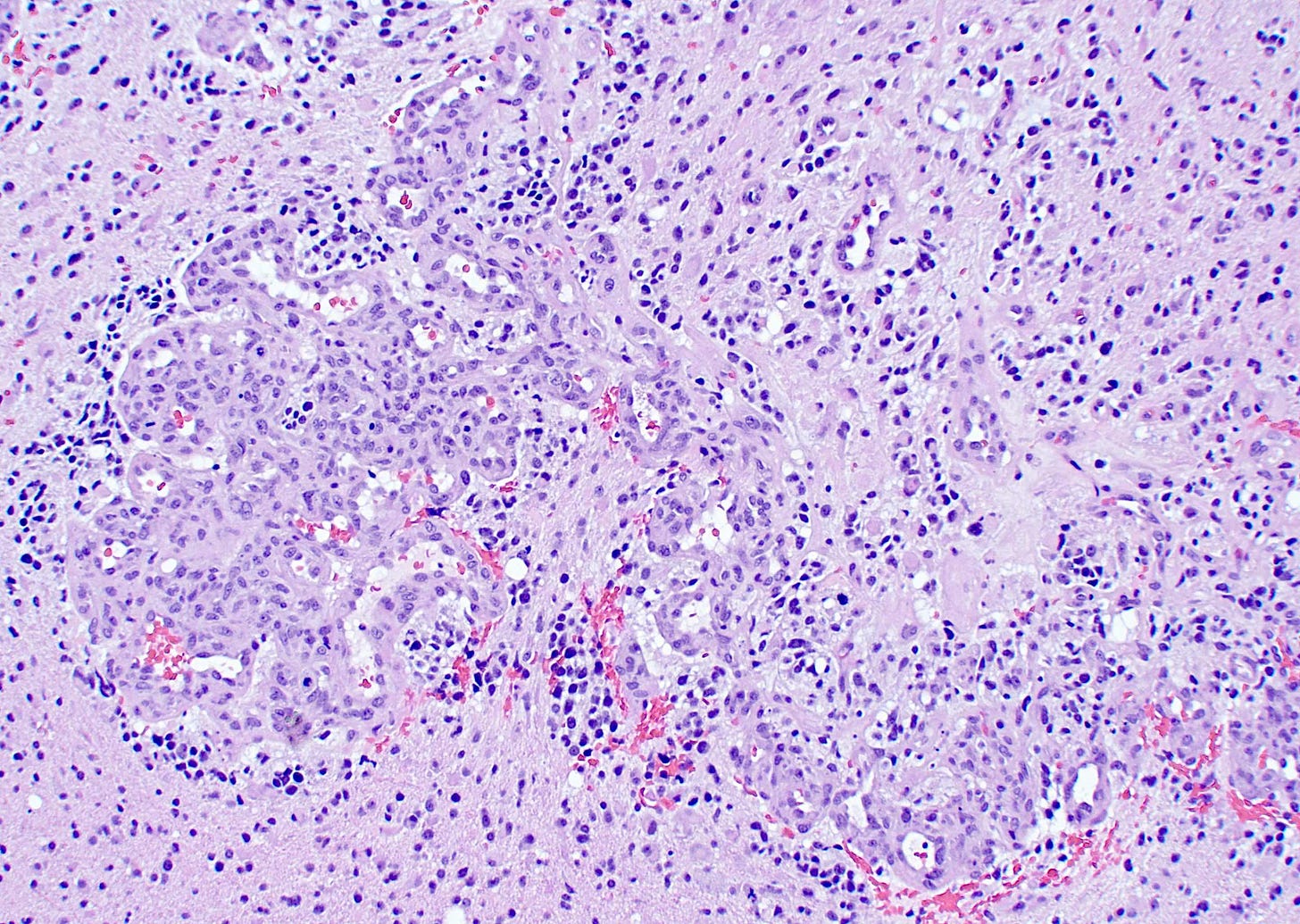
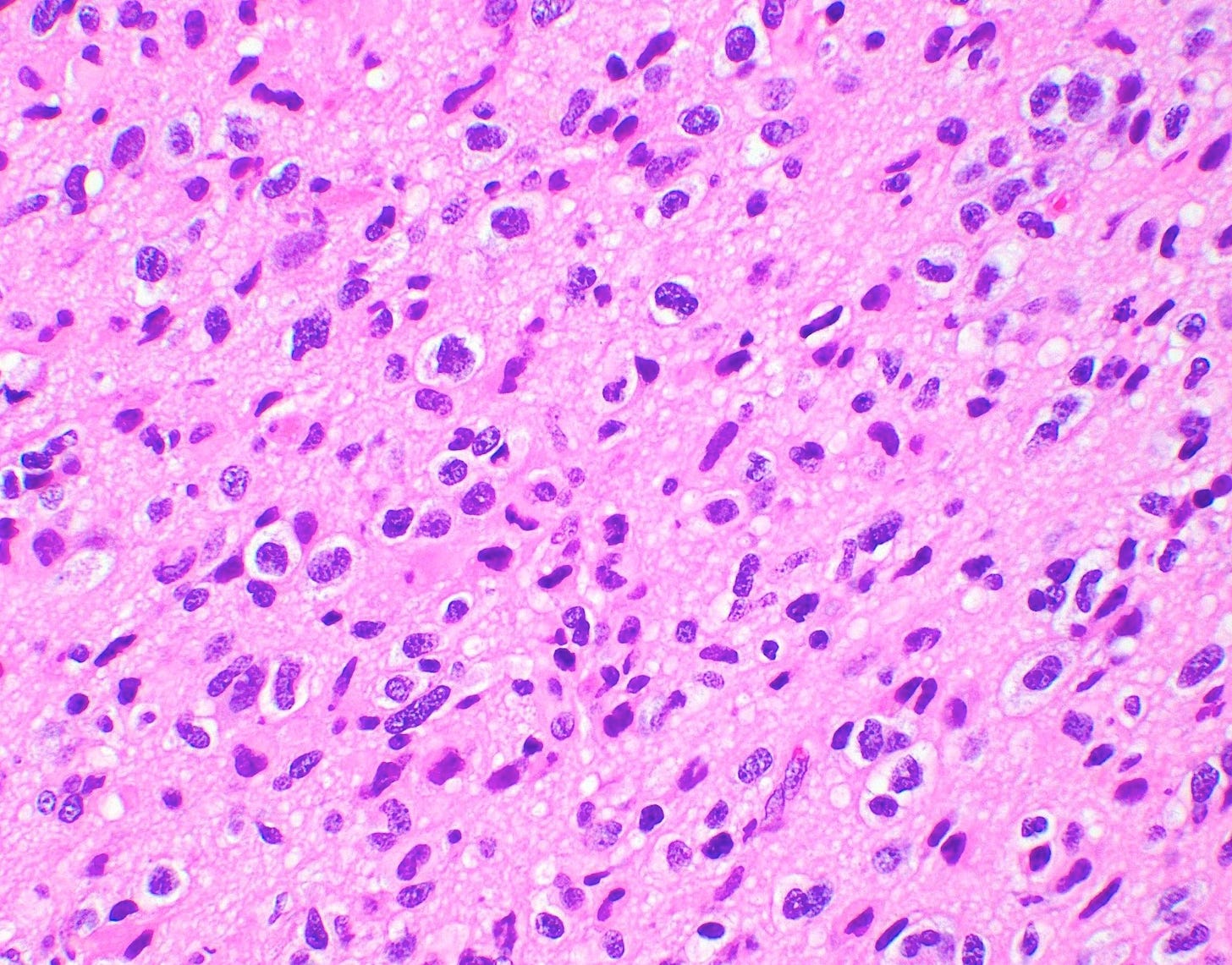
Glioblastoma may begin with a stem or progenitor cell that contains the defining molecular changes of EGFR amplification, TERT mutations or copy number changes in the form of a combined gain of chromosome 7 and loss of chromosome 10. Alternatively, there may be molecular changes to other networks that initiate the defining histologic changes of brisk mitotic activity and microvascular proliferation or necrosis. These molecular changes may promote genomic instability so that dividing cells acquire additional molecular changes or mutations that further the malignant process until a clinically evident tumor is identified. For this scenario, none of these steps would be considered a morphologic precursor.

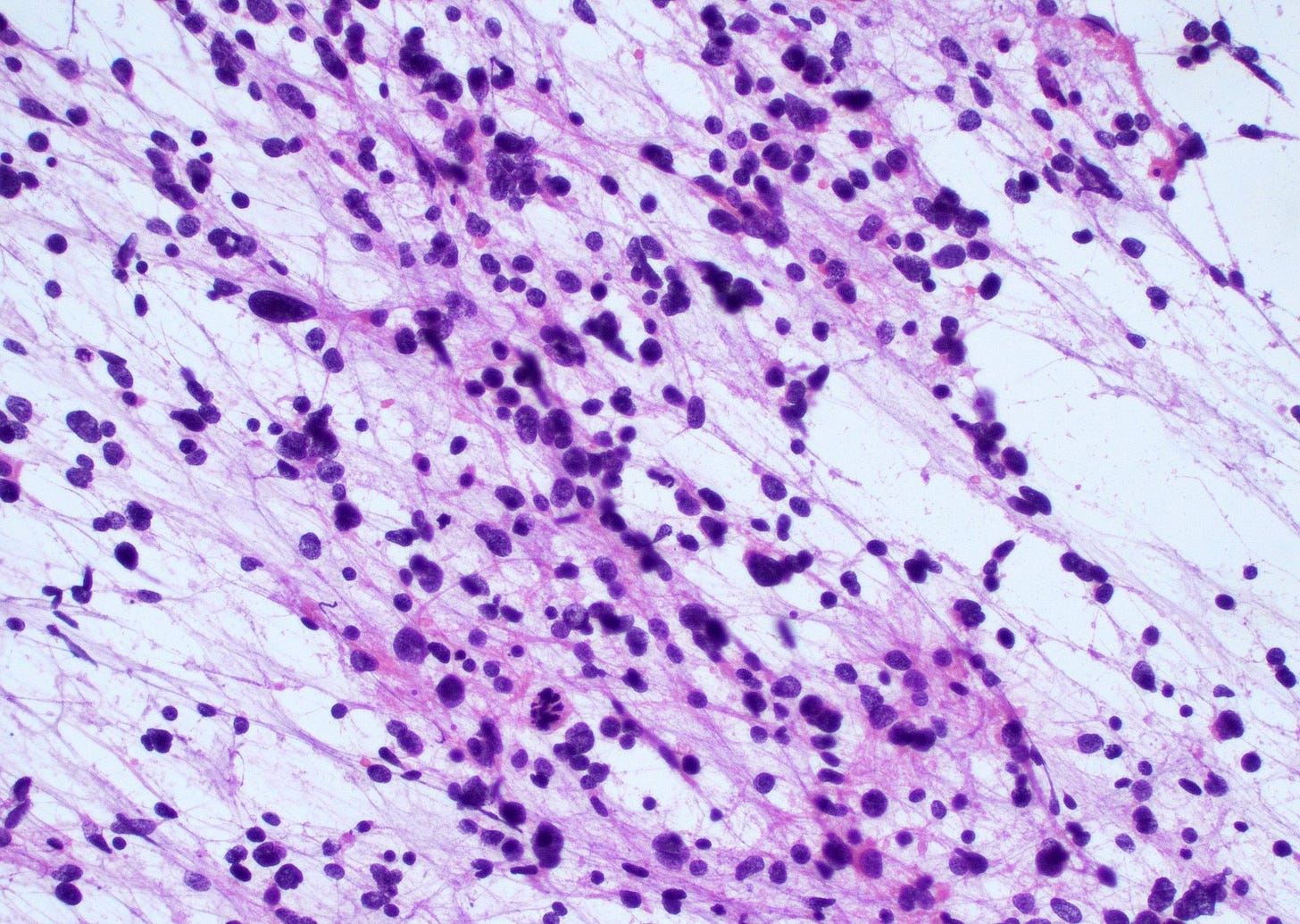
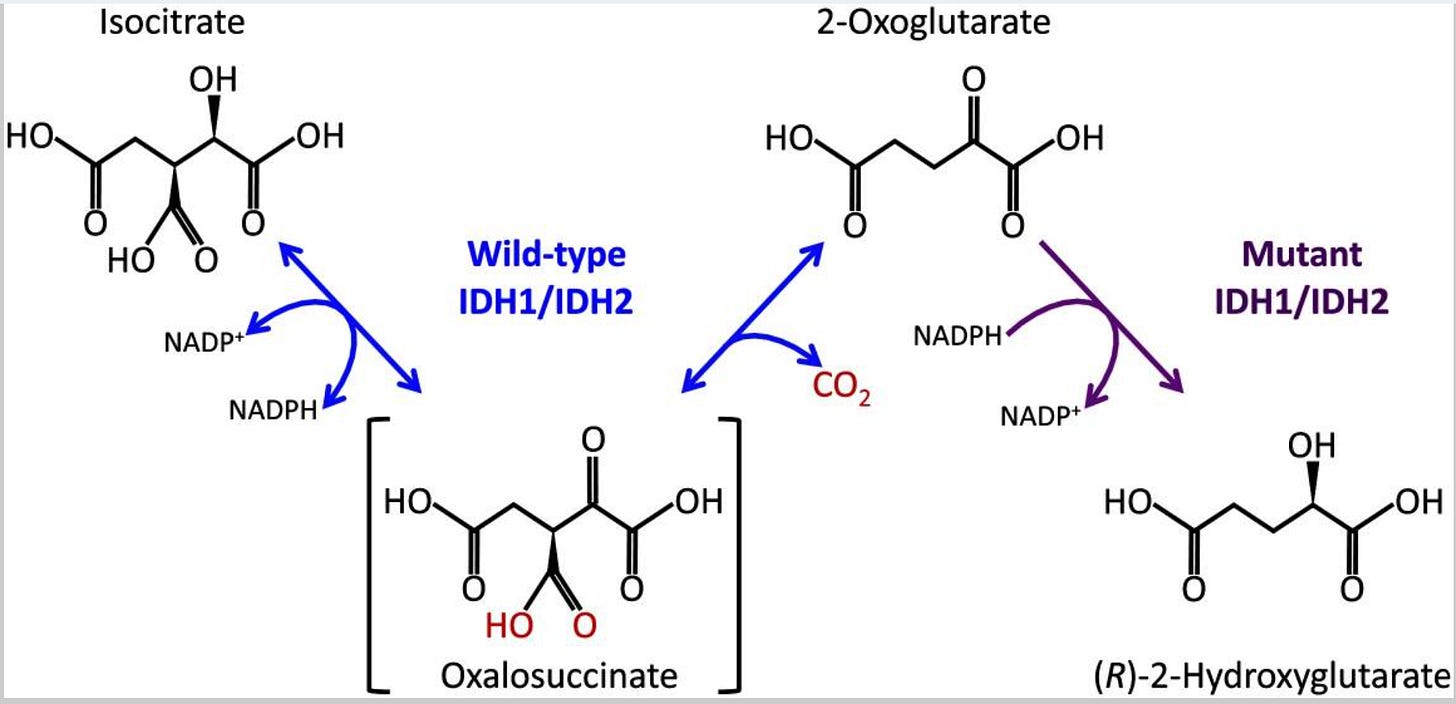
Similarly, oligodendroglioma, a relatively uncommon brain tumor, has defining mutations in both IDH1 or IDH2 and 1p / 19q whole arm codeletions. These IDH mutations create an enzyme that generates a metabolite not normally detectable in the brain (Exner 2019). The metabolite disrupts the function of proteins involved in epigenetic modification and interrupts the differentiation process. The IDH mutation appears to be a gatekeeper that triggers uncontrolled proliferation, which renders cells vulnerable to additional mutations that further the malignant process until a clinically evident tumor is identified; however, as with glioblastoma, none of these steps would be considered a morphologic precursor.
Pituitary hyperplasia, particularly in familial cases, may theoretically be a precursor to pituitary neuroendocrine tumors, analogous to how endocrine cell hyperplasia is a precursor to stomach neuroendocrine tumors, but adequate evidence is lacking.
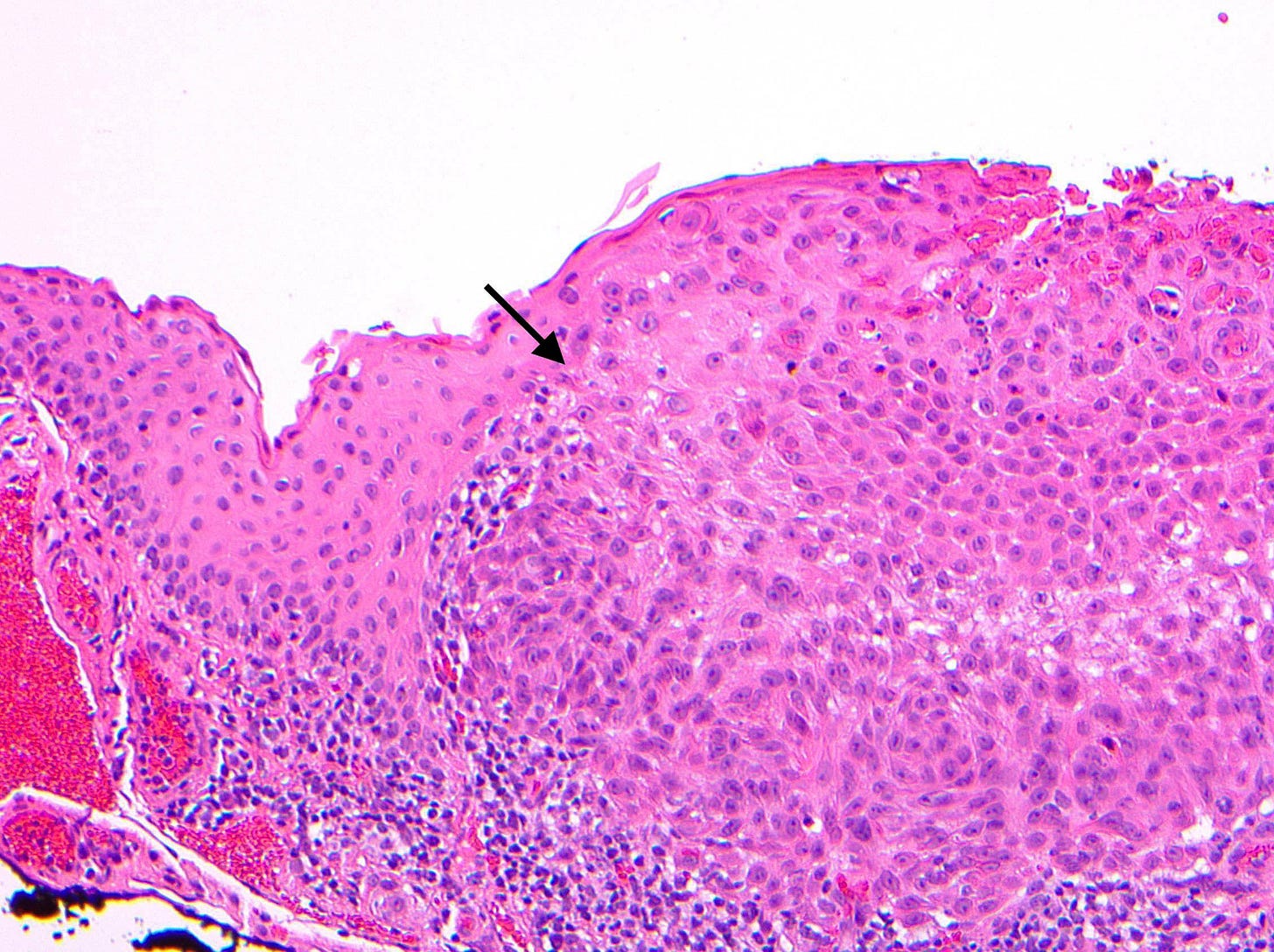
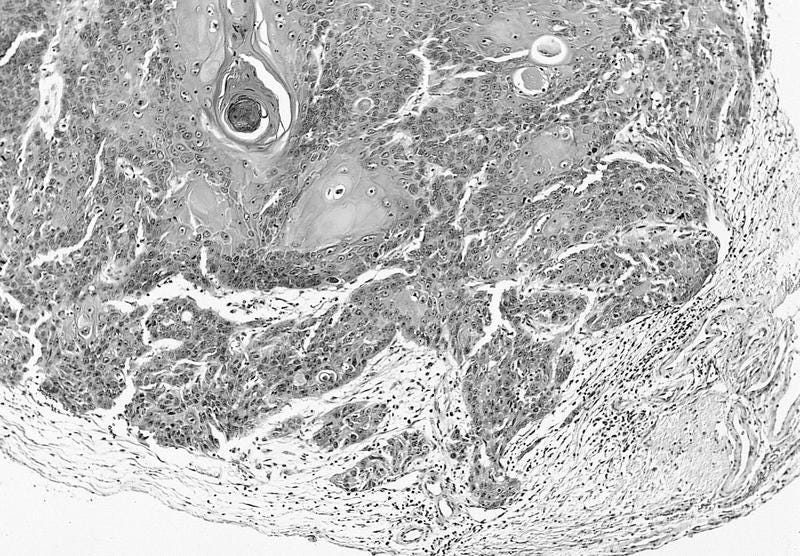
In the eye, we have only identified one precursor: conjunctival intraepithelial neoplasia, which may lead to conjunctival squamous cell carcinoma and follows the classic intraepithelial neoplasia pathway described previously for carcinomas.
Part 3 will discuss precursors associated with skin malignancies.
If you like these essays, please subscribe or share them with others.
Click here for the Index to Nat’s blog on Cancer and Medicine
Follow us on Substack, LinkedIn, Threads and Instagram (npernickmich) and Tribel (@nat385440b).
Follow our Curing Cancer Network through our Curing Cancer Newsletter, on LinkedIn or Twitter or the CCN section of our PathologyOutlines.com blog. Each week we post interesting cancer related images of malignancies with diagnoses plus articles of interest. Please also read our CCN essays.
Latest versions of our cancer related documents:
American Code Against Cancer (how you can prevent cancer)
Email me at Nat@PathologyOutlines.com - Unfortunately, I cannot provide medical advice.
I also publish Notes at https://substack.com/note. Subscribers will automatically see my Notes.




