Cancer precursor project - characteristics of premalignant precursors, part 5b (hematopathology)
23 June 2024, revised 2 July 2024
Our Cancer precursor project aims to better understand how cancer arises by compiling a regularly updated spreadsheet of all distinct human cancers (now 1,229) and their precursors (now 171).
Please subscribe to this free blog on Cancer and Medicine (posted every 1 - 2 weeks) and to our free Curing Cancer Network newsletter (posted every 1 - 2 months).
Hematologic malignancies only rarely have precursors. We have identified only 6 precursors associated with 207 distinct hematologic malignancies (i.e., leukemias and lymphomas arising in the bone marrow and lymphoid tissue) and these precursors typically are either not morphologic (meaning the cancer cells do not appear different microscopically between the precursor and the malignancy) or are rare. In part 5a, we discussed
1. Plasma cell myeloma (multiple myeloma): precursor is monoclonal gammopathy of undetermined significance (MGUS) - differences are clinical, not morphologic
2. Lymphoplasmacytic lymphoma: occasionally has MGUS IgM as a precursor -differences are clinical, not morphologic
3. Chronic lymphocytic leukemia (CLL) / small lymphocytic lymphoma (SLL): precursor is B cell monoclonal lymphocytosis - differences are clinical, not morphologic
In part 5b, we discuss
4. Follicular lymphoma: rarely has follicular neoplasia in situ as a precursor
5. Mantle cell lymphoma: rarely has in situ mantle cell neoplasia as a precursor
6. Enteropathy associated T cell lymphoma: commonly has celiac disease with villous atrophy and increased intraepithelial T lymphocytes as a precursor
4. Follicular neoplasia in situ as a precursor for follicular lymphoma
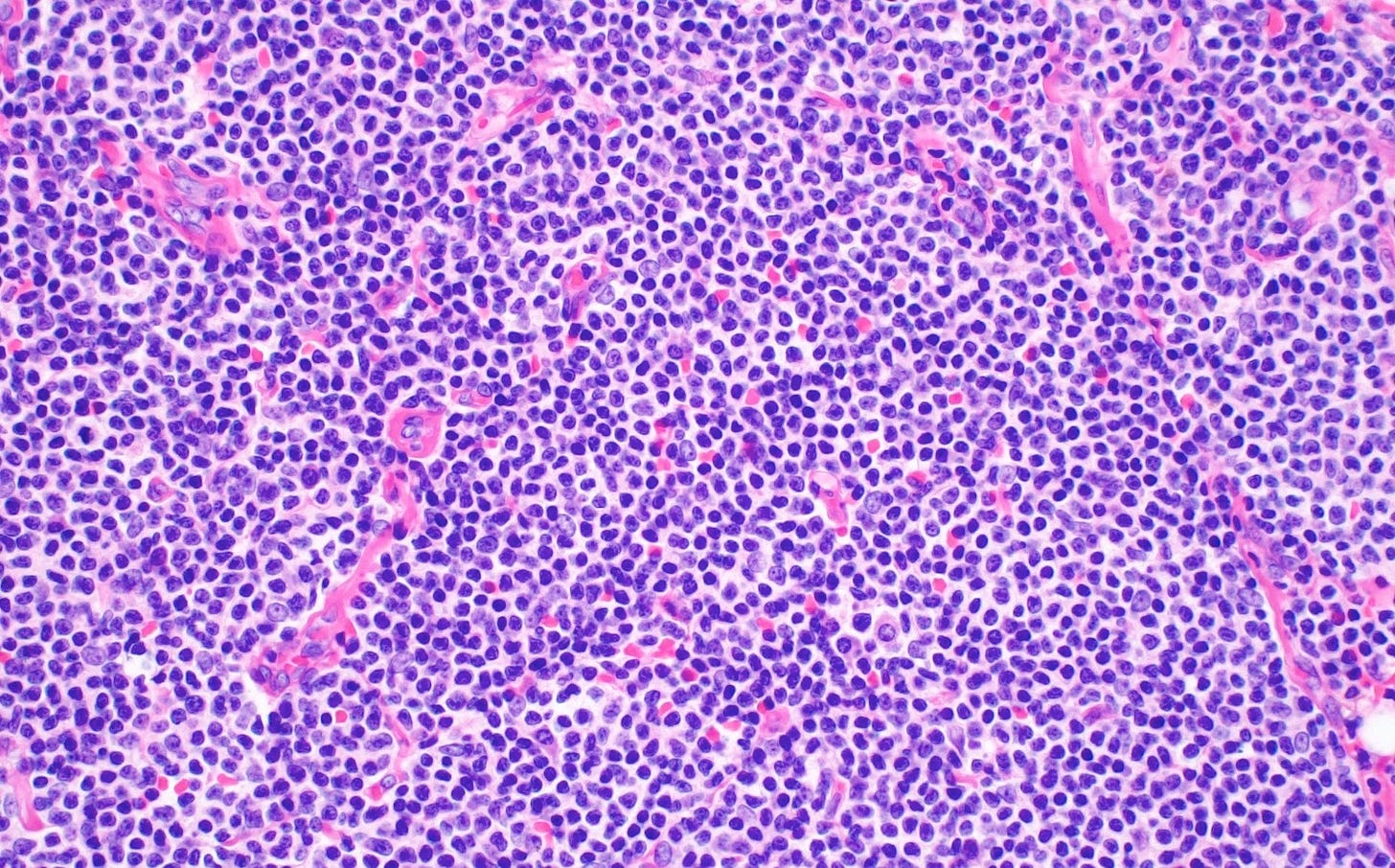
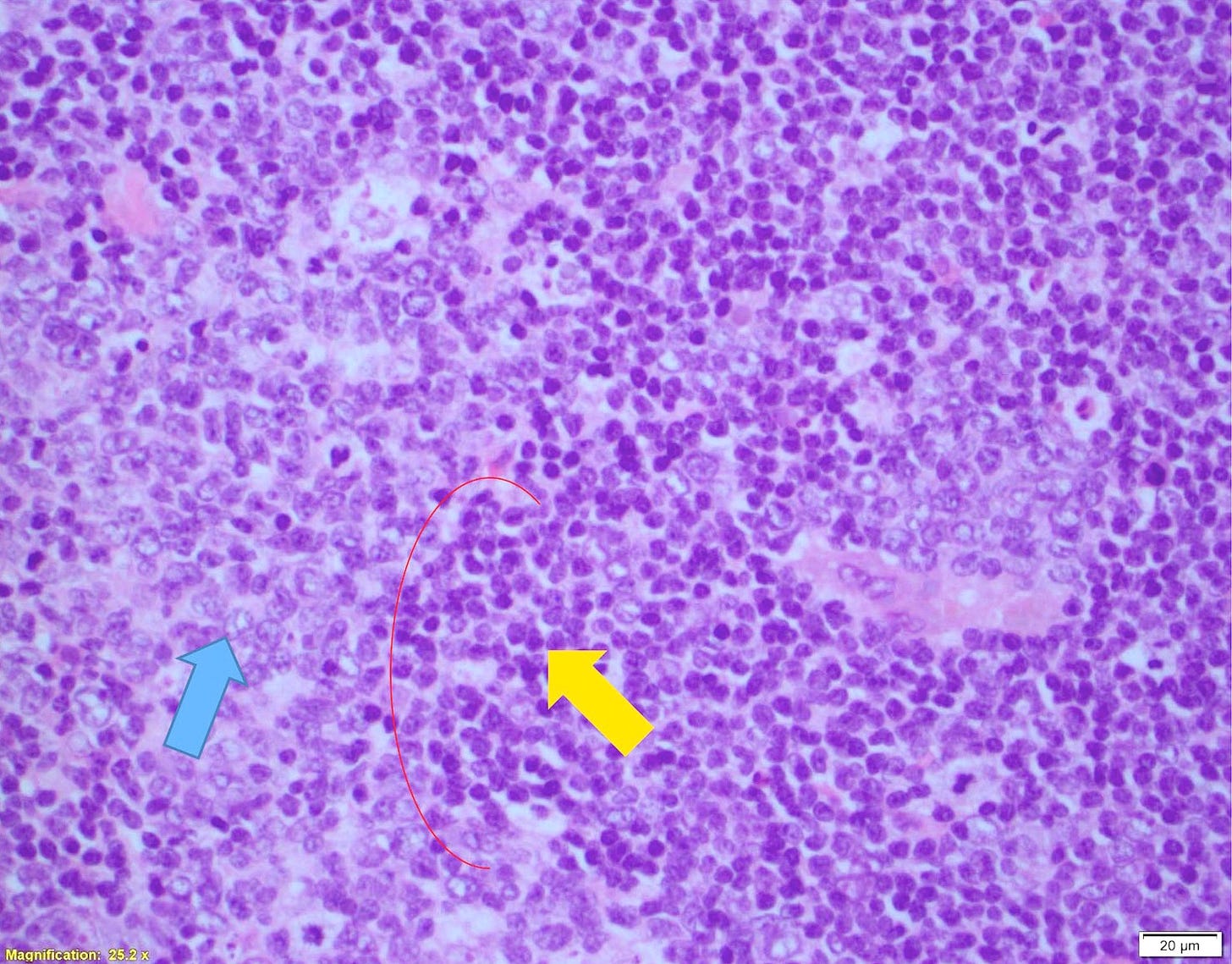
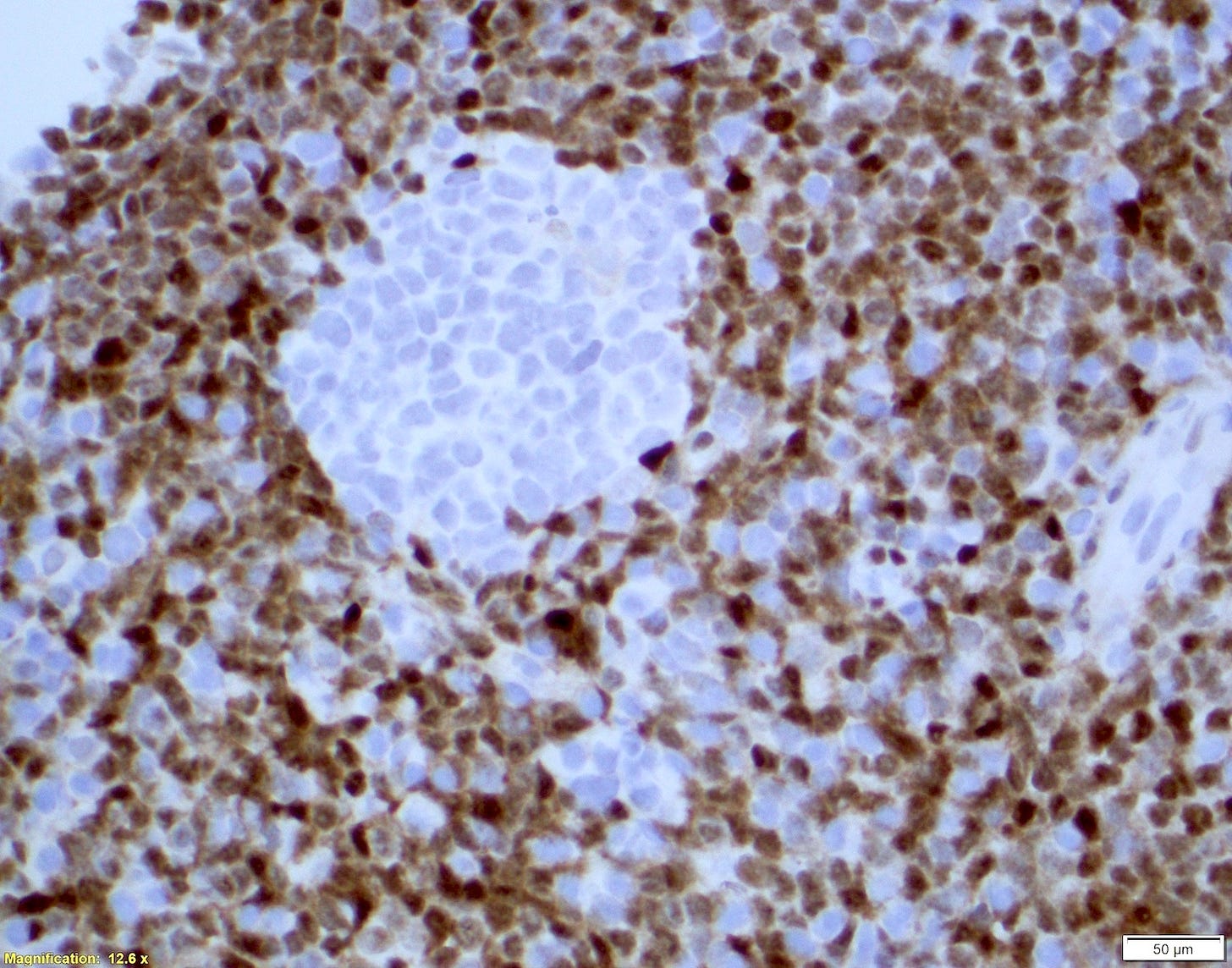
Follicular neoplasia in situ is a monoclonal proliferation of B lymphocytes (B cells) confined to follicle centers of the lymph node, which preserves the lymph node architecture. The B cells are BCL2 positive and contain t(14;18)(q32;q21), the classic translocation of follicular lymphoma (a translocation is when pieces of two chromosomes break off and switch places with each other). By definition, clinical and pathological evidence of follicular lymphoma is lacking. Since only rare cases (< 5%) progress to follicular lymphoma, no treatment is indicated other than follow up. It may arise from a different and less aggressive malignant pathway than most cases of follicular lymphoma.
Follicular neoplasia in situ


Follicular lymphoma is the second most common non-Hodgkin lymphoma after diffuse large B cell lymphoma. It accounts for 20 - 25% of all new non-Hodgkin lymphoma diagnoses in Western countries. The average age at diagnosis is 60 - 65 years. At diagnosis, it typically is localized and indolent and affects the cervical and inguinal lymph nodes. Untreated cases may subsequently involve the bone marrow, spleen, liver and peripheral blood. In 1979 - 1983, when I was a medical student, it had no treatment and patients would be followed until the lymphoma progressed to diffuse large B cell lymphoma, which would then be treated. Today, patients with indolent, localized disease are treated with radiation therapy and Rituximab, a monoclonal antibody to B cells; most patients now live > 15 years.
Most follicular lymphoma cases have no known cause. Only rare cases have follicular neoplasia in situ as a precursor. Follicular lymphoma is strongly associated with the molecular translocation of t(14;18)(q32;q21), which arises during antibody production (Roth 2016); however, this change is insufficient to cause lymphoma by itself (Mamessier 2014). Multiple additional molecular changes are needed for the cell to possess clinically malignant properties.
Follicular lymphoma


5. In situ mantle cell neoplasia as a precursor for mantle cell lymphoma
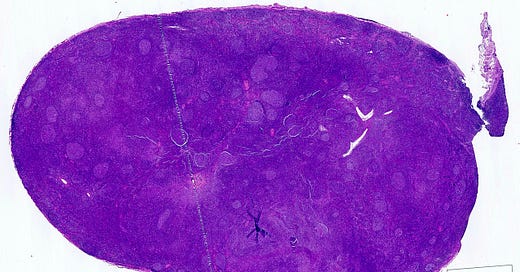
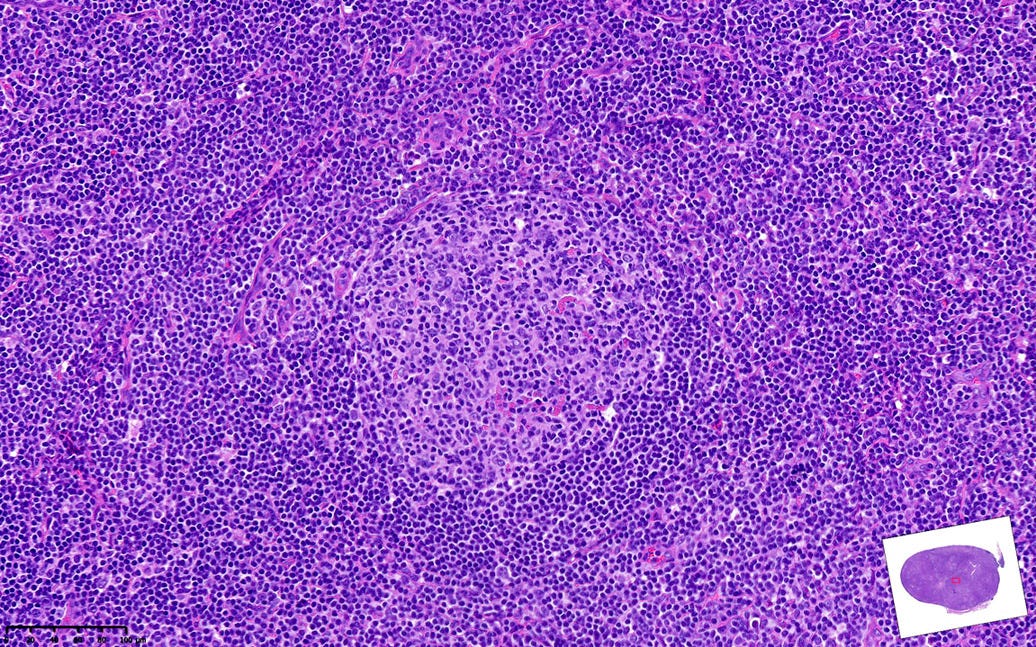
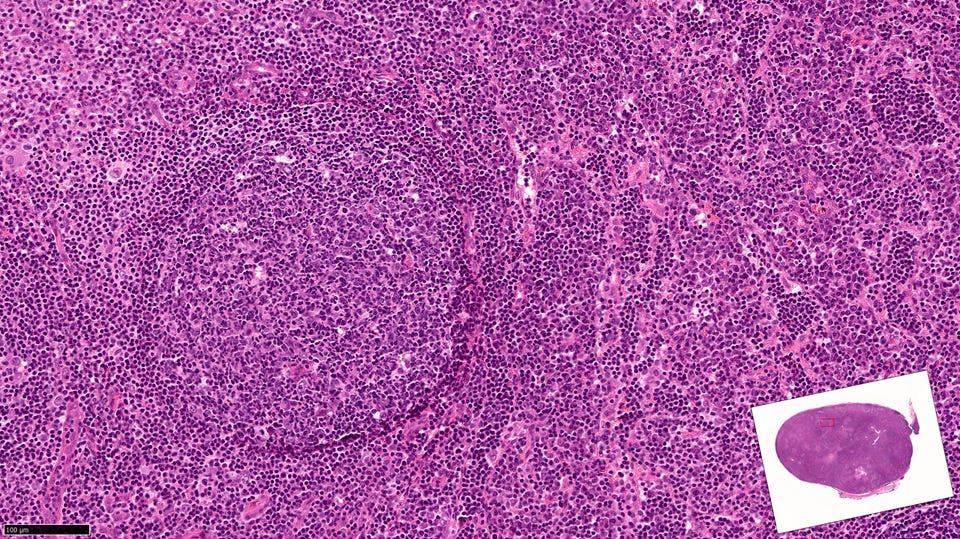
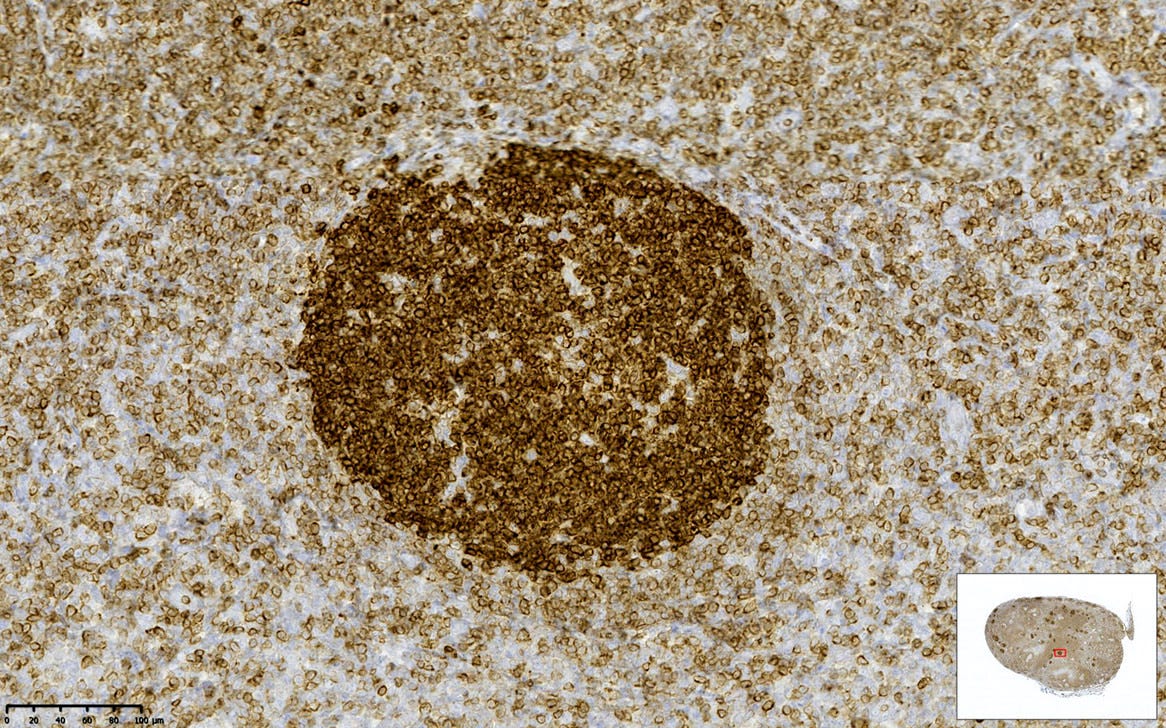
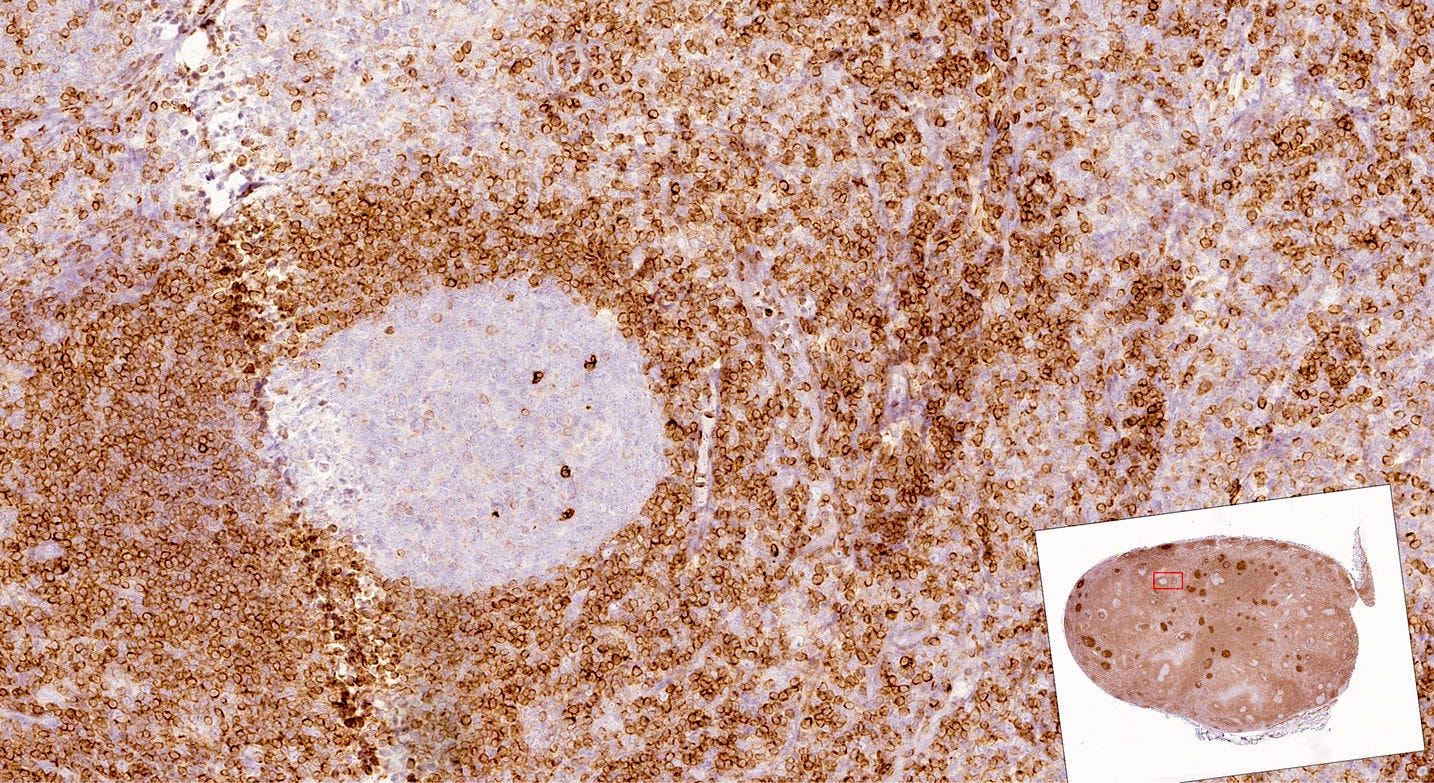
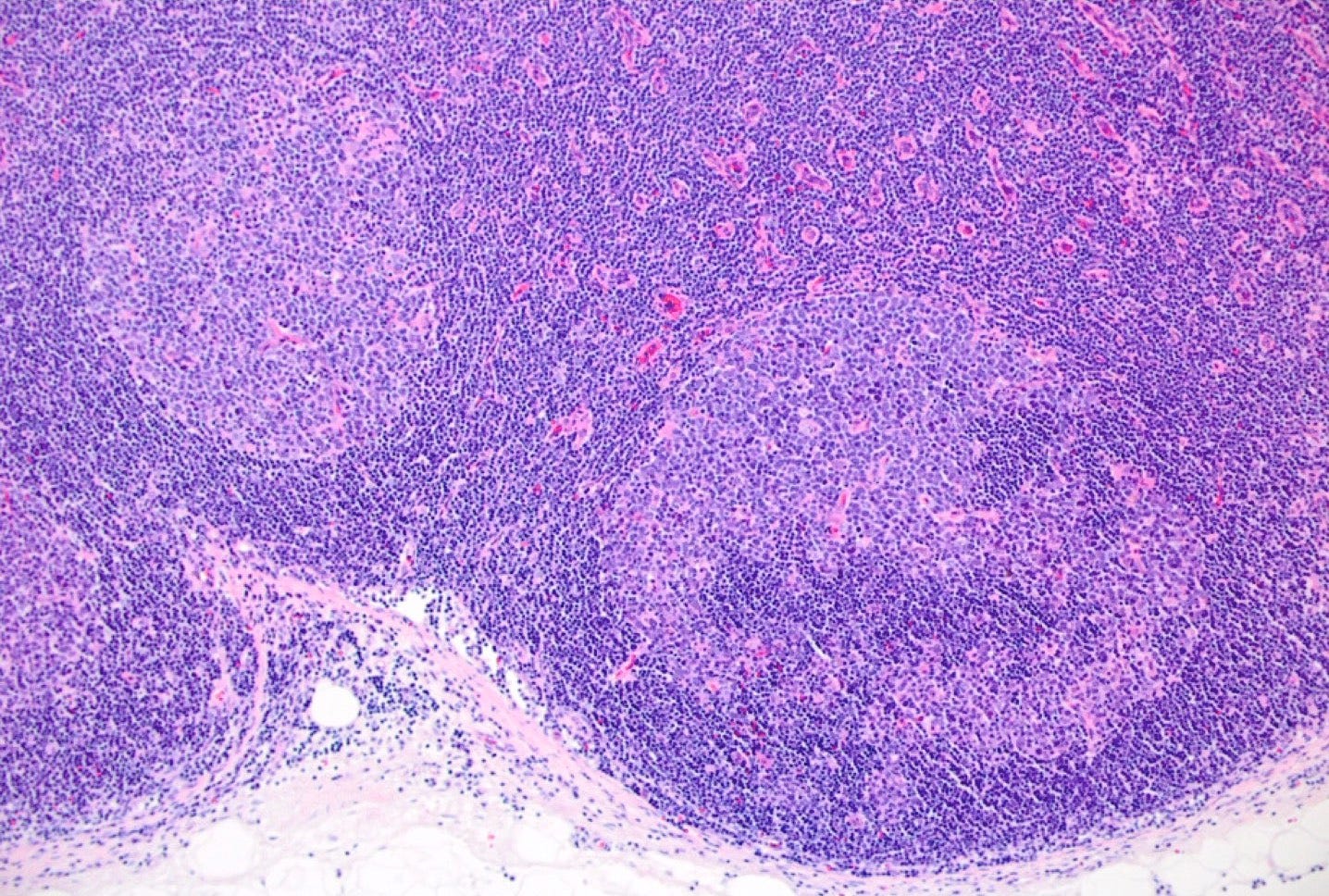
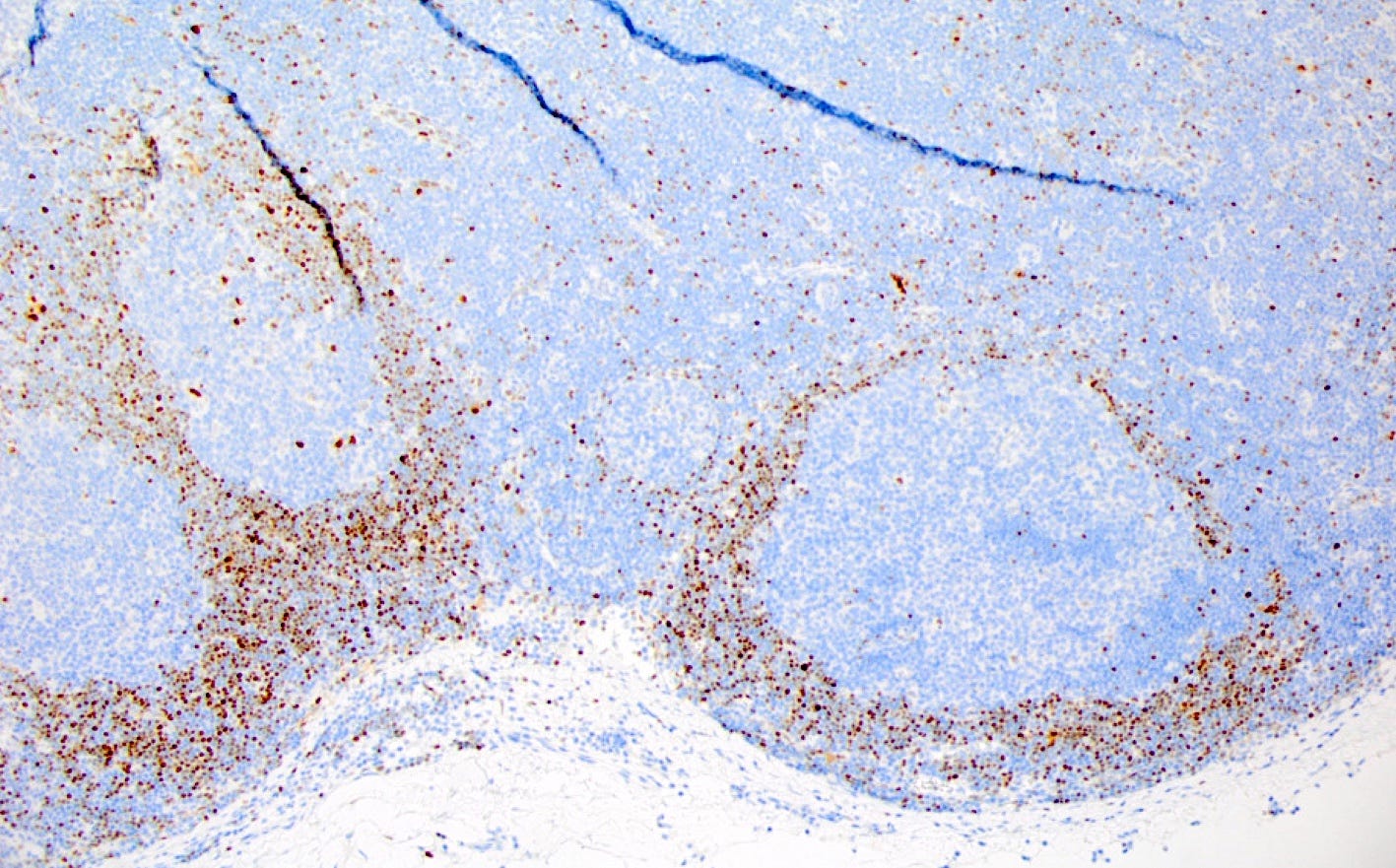
In situ mantle cell neoplasia is rarely a precursor of mantle cell lymphoma. It usually presents as an incidental finding of a reactive appearing lymph node with a normal lymph node architecture and no or only slight mantle zone expansion. The mantle zones are composed of cyclin D1 positive B cells with CCND1 rearrangements restricted to the mantle zones. Typically, it is a stable disease with indolent behavior and long term survival, even without treatment. It progresses to mantle cell lymphoma in < 10% of cases.
In situ mantle cell neoplasia
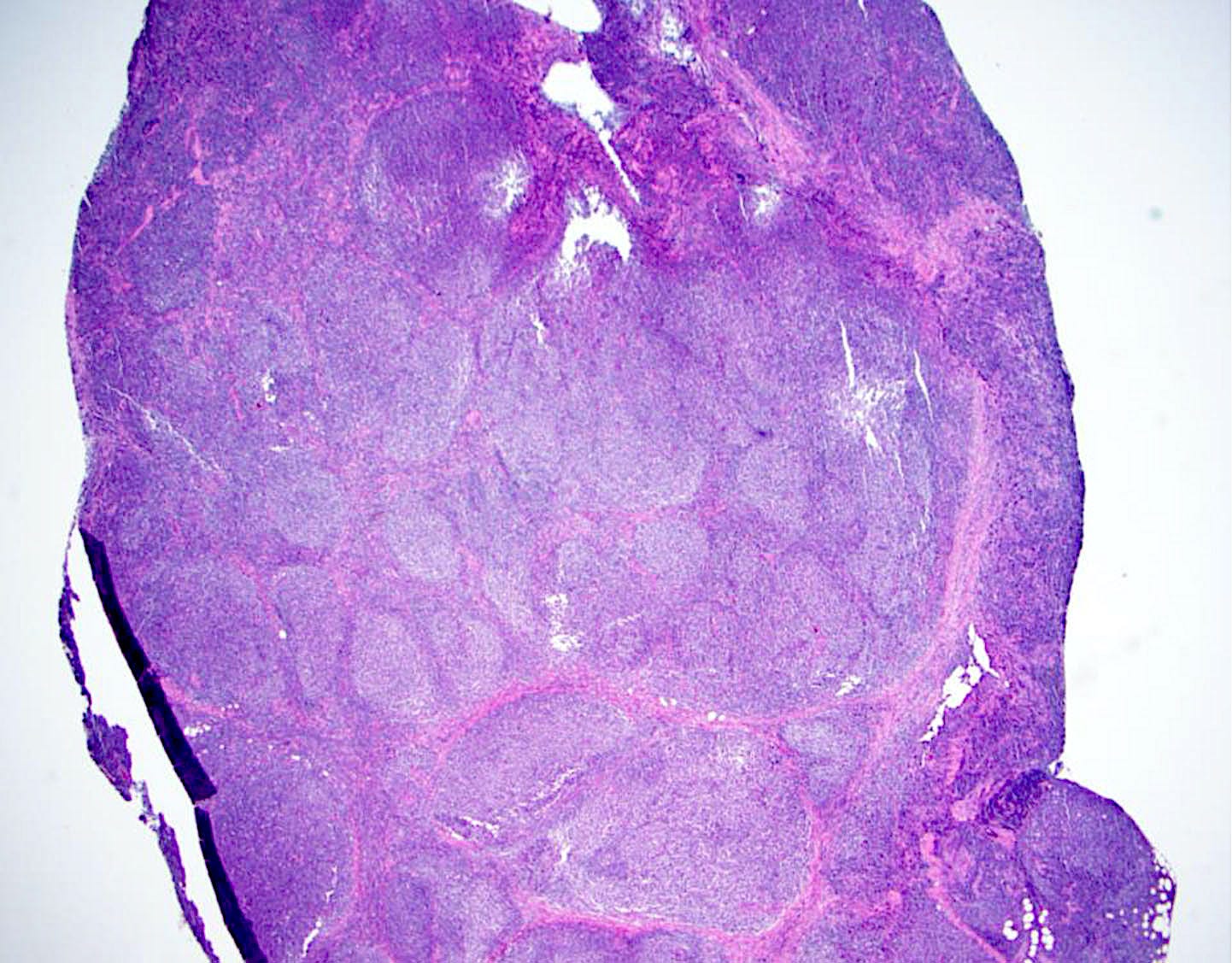
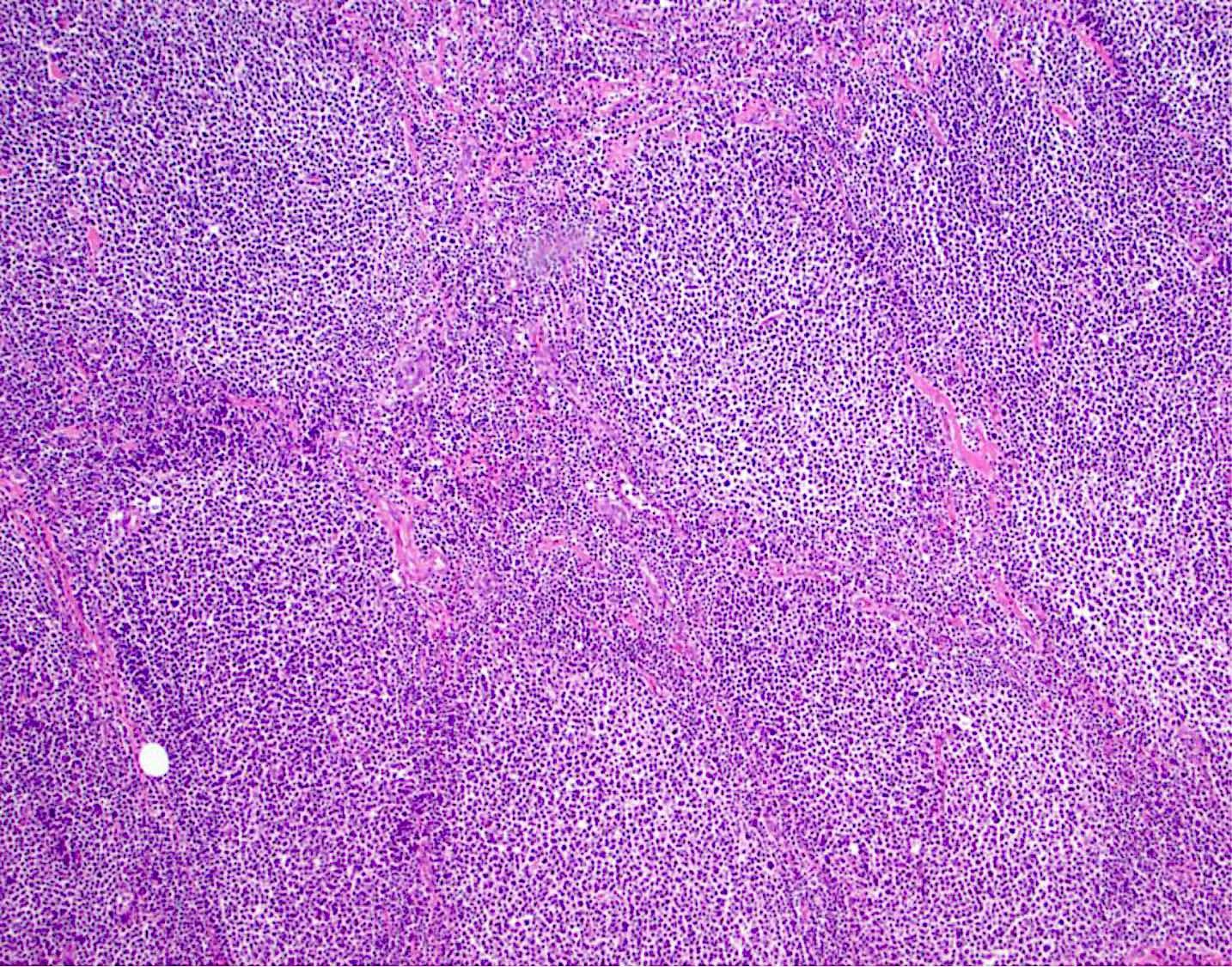
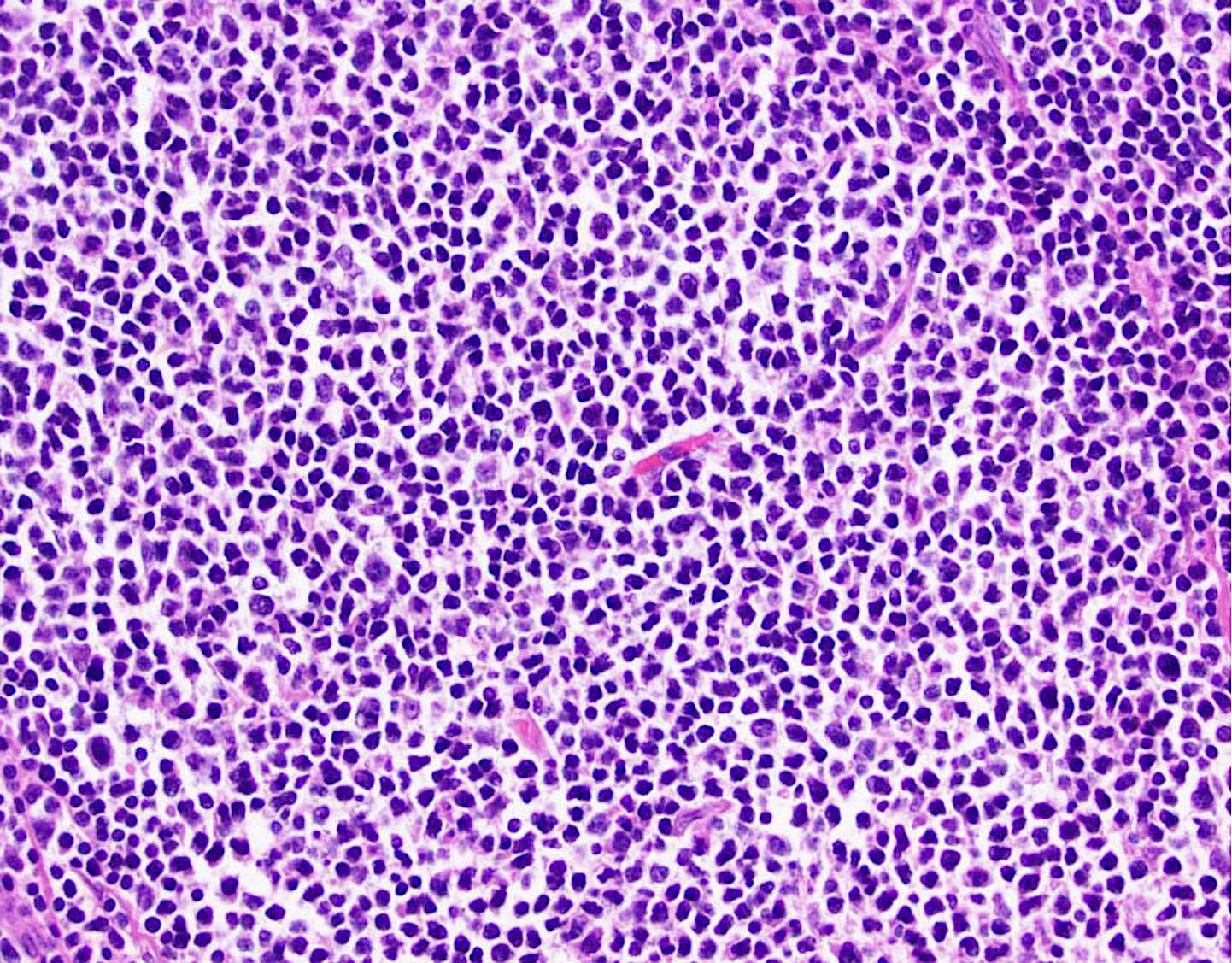
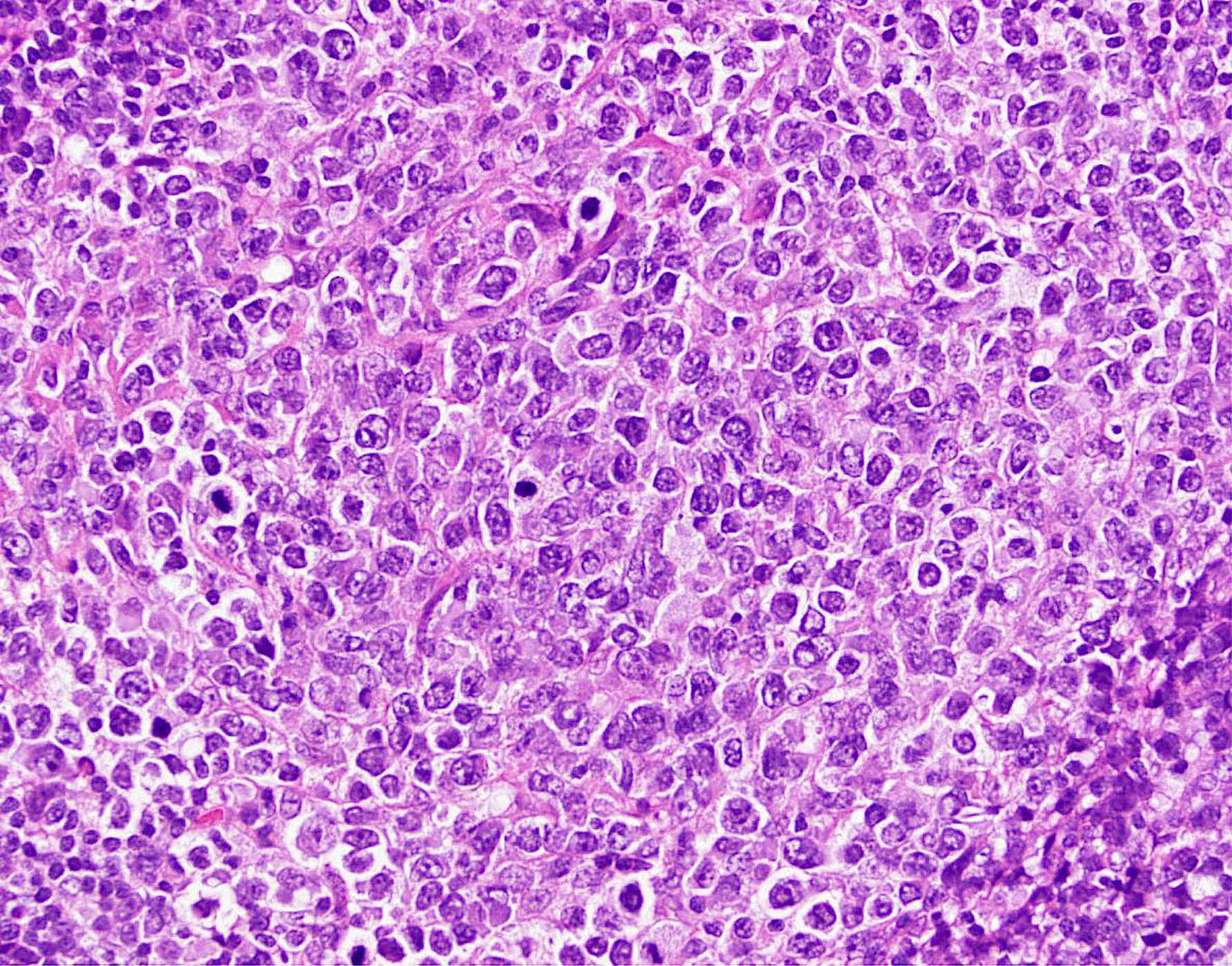
Mantle cell lymphoma is a clinically aggressive B cell lymphoma comprising ~10% of non-Hodgkin lymphomas. The median age (50th percentile) is 68 years and two - thirds of patients are men. Mantle cell lymphoma is composed of small to medium sized lymphoid cells that are typically monomorphic and almost all cases have the t(11;14)(q13;q32) or translocation of the IGH / CCND1 genes with cyclin D1 overexpression, which leads to the dysregulation of the cell cycle. It is treated with aggressive chemotherapy and the median survival is 5 - 7 years.
Mantle cell lymphoma
6. Celiac disease as a precursor for enteropathy associated T cell lymphoma
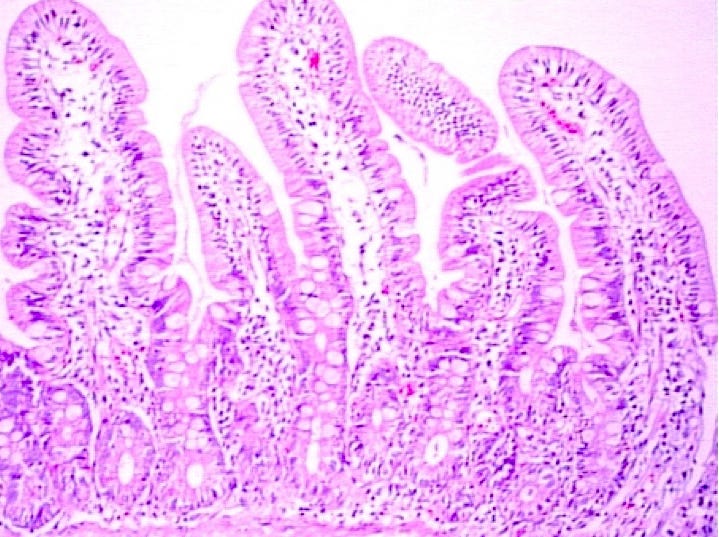
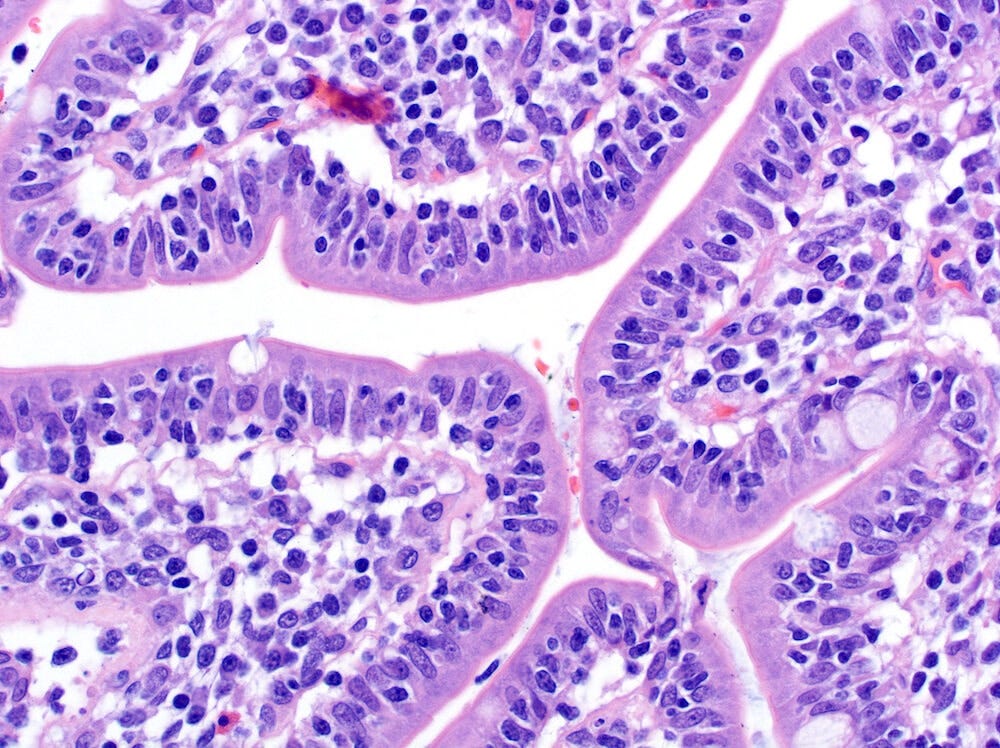
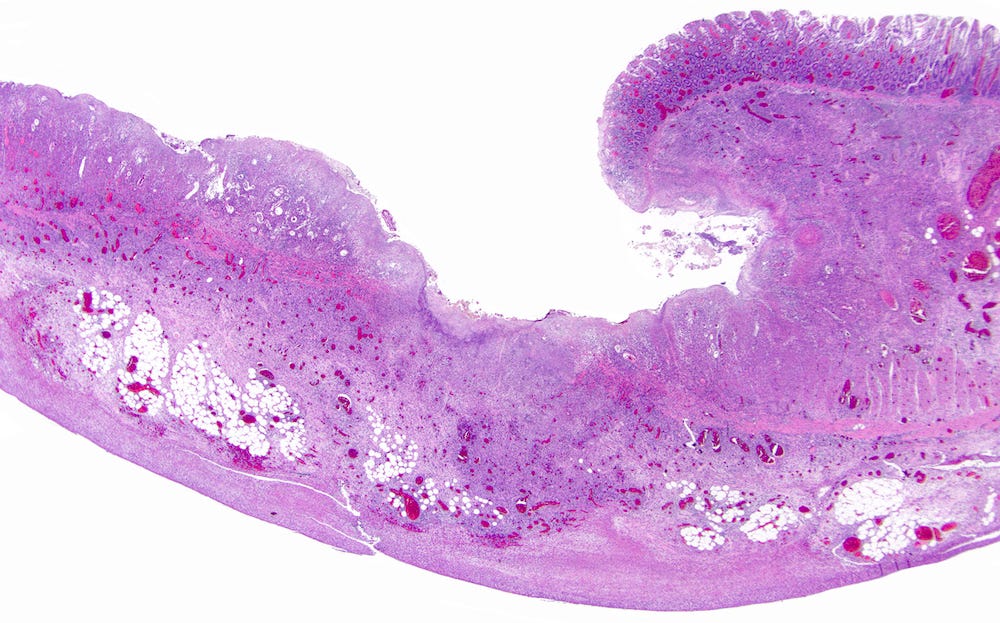
Celiac disease (celiac sprue, gluten sensitive enteropathy) causes a malabsorption syndrome with chronic diarrhea, weight loss and asthenia (physical weakness or lack of energy). Celiac disease is an immune mediated inflammatory disease of the small intestine. It is found in genetically predisposed individuals and is caused by sensitivity to prolamins (a type of plant storage protein) including wheat (gliadin), barley, rye and oats. The innate and adaptive immune response to prolamins leads to chronic inflammation of the small intestinal epithelium (intraepithelial T cell lymphocytosis), villous atrophy and ultimately malabsorption.
Treatment consists primarily of a gluten free diet, which typically resolves the symptoms and the microscopic findings; however, patients with refractory celiac disease type 2 with shortened villi have persistent malabsorption and are at risk for enteropathy associated T cell lymphoma. This lymphoma also occasionally occurs in those with long lasting, well controlled celiac disease.
Celiac disease


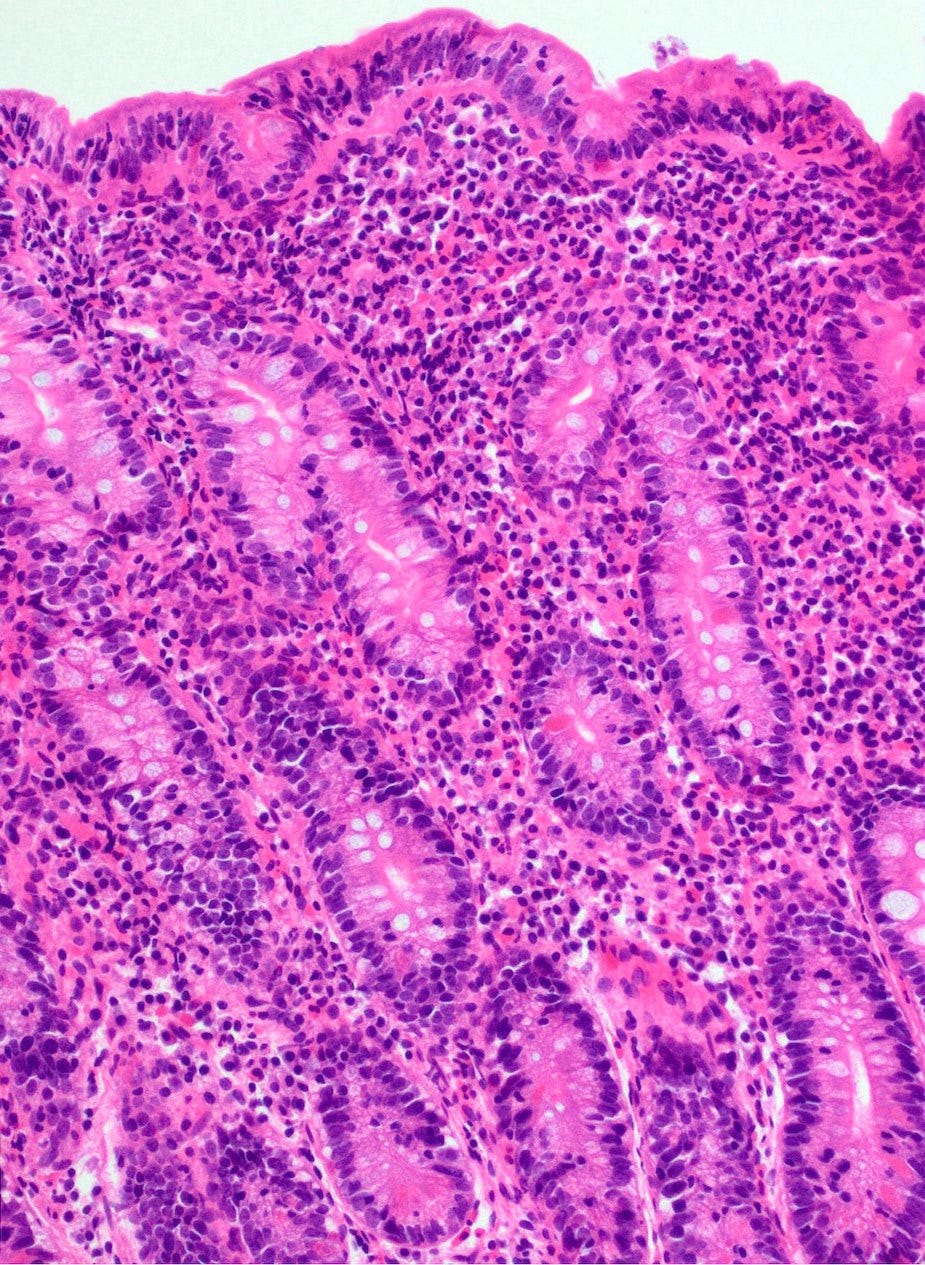
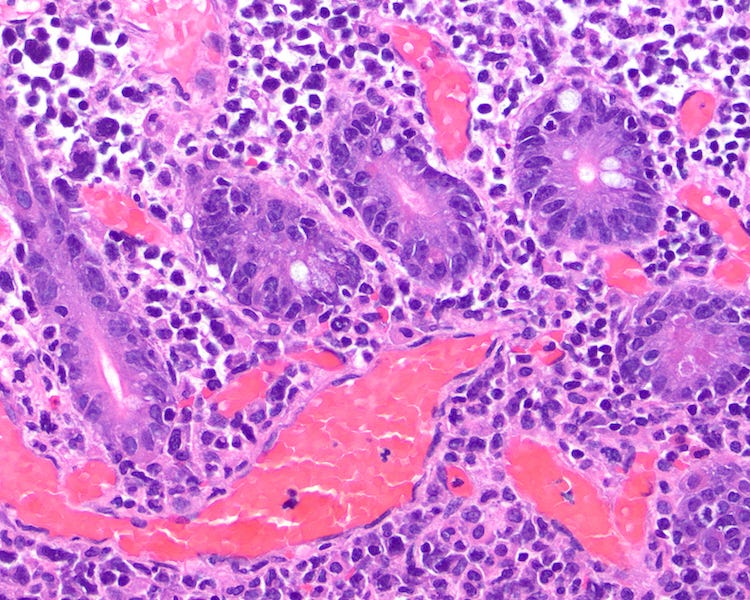
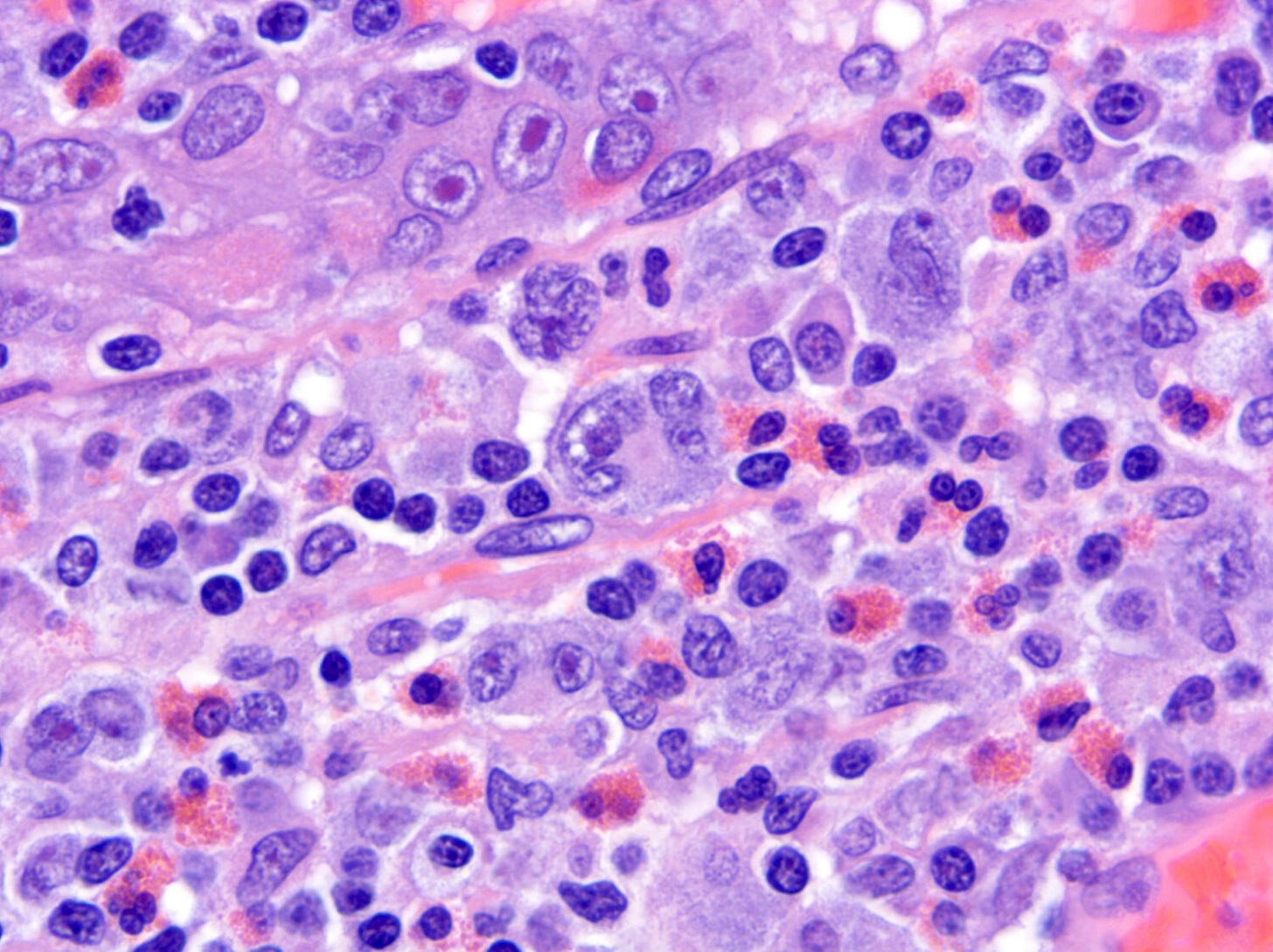
Enteropathy associated T cell lymphoma is an intestinal lymphoma derived from intraepithelial T cells. It is rare, constituting < 1% of all non-Hodgkin lymphomas and typically affects the small intestine. Patients are usually in their 50s or 60s and from Western countries.
Enteropathy associated T cell lymphoma has a strong association with refractory celiac disease (i.e., celiac disease that does not respond to at least 12 months of gluten free diet) and typically is diagnosed 5 - 10 years after the diagnosis of celiac disease. It arises due to the inherent instability of lymphocytes. The persistent activation of lymphocytes in different clinical conditions ultimately may cause lymphoma, including MALT lymphoma in B cells of the stomach due to chronic Helicobacter pylori infection or enteropathy associated T cell lymphoma in T cells of the small intestine due to the autoimmunity associated with celiac disease.
Enteropathy associated T cell lymphoma often presents with GI symptoms and infections and sometimes is diagnosed at the same time as celiac disease. It is aggressive and has a 5 year survival of only 20%.
Enteropathy associated T cell lymphoma
Our initial essays focused on the 4 subspecialties (neuropathology; bone, joints & soft tissue; hematopathology; dermatopathology) whose malignancies only rarely had malignancies (17 precursors for 540 malignancies or 3.1%). Next we will focus on the epithelial malignancies with known precursors.
If you like these essays, please subscribe or share them with others. These essays will continue to be free. Instead of requesting money, we hope you repost these essays and strive to make our world a better place and yourself a better person.
Click here for the Index to Nat’s blog on Cancer and Medicine
Follow us on Substack, LinkedIn, Threads and Instagram (npernickmich) or Tribel (@nat385440b).
Follow our Curing Cancer Network through our Curing Cancer Newsletter, on LinkedIn or Twitter or the CCN section of our PathologyOutlines.com blog. Each week we post interesting cancer related images of malignancies with diagnoses plus articles of interest. Please also read our CCN essays.
Latest versions of our cancer related documents:
Strategic plan to substantially reduce cancer deaths (June 2023)
American Code Against Cancer (how you can prevent cancer) (January 2023)
Cancer Precursor Project spreadsheet (May 2024) and General Overview (May 2024)
Email me at Nat@PathologyOutlines.com. Unfortunately, I cannot provide medical advice.
I also publish Notes at https://substack.com/note. Subscribers will automatically see my Notes.