Cancer precursor project - characteristics of premalignant precursors, part 5a (hematopathology)
13 June 2024
Our Cancer precursor project aims to understand better how cancer arises by compiling a regularly updated spreadsheet of all distinct human cancers (now 1,229) and their precursors (now 171).
We invite you to subscribe to these free essays as well as to our free Curing Cancer Network newsletter (posted every 1-2 months).
In part 1, we discovered that the percentage of identified precursors varies widely by pathology subspecialty and we discussed precursors in subspecialties with epithelial sites (breast, head & neck, gyn, GI / liver, GU / adrenal and thoracic). This is the current version of this table:
In part 2, we discussed neuropathology related malignancies and their lack of precursors and concluded that contrary to current thinking, most nonepithelial malignancies, including central nervous system tumors, lack precursors.
In parts 3a and 3b, which discuss skin malignancies, we proposed that there are three general malignant processes. First, many malignancies may be initiated by a defining mutation in a single stem or progenitor cell that multiplies and acquires additional mutations and malignant properties over time but without any morphologic precursor.
Second, in the skin and other sites with epithelium, the single cell malignant process may be inhibited by epithelial cell - cell interactions and its basement membrane, which forces it to go through the additional steps of intraepithelial neoplasia. Third, we speculated that some skin malignancies may have a precursor with distinct molecular patterns somewhat similar to the intraepithelial neoplasia process but with no easily identifiable morphologic changes, although this has not been proven.
In part 4, we noted that of the 140 distinct bone and soft tissue tumors identified, only 4 had premalignant precursors, which were rare except when associated with syndromic or genetic disorders. We also revised our spreadsheet to exclude malignant precursors.
In parts 5a and 5b, we discuss precursors associated with hematologic malignancies (i.e., leukemias and lymphomas arising in the bone marrow and lymphoid tissues). We have identified only 6 precursor conditions out of 207 distinct diagnoses but because the cells of the precursors and the malignancies appear similar microscopically, some of these precursors (MGUS, B cell monoclonal lymphocytosis) might be better considered as clinical precursors rather than morphologic precursors.
1. Plasma cell myeloma (multiple myeloma): almost all cases arise in patients with precursor monoclonal gammopathy of undetermined significance (MGUS) (85% non-IgM, 15% IgM); however, the differences between MGUS and myeloma are clinical, not morphologic (i.e., the plasma cells appear similar in both). MGUS has a lower serum M protein of < 30 g/L (3 g/dL), < 10% bone marrow clonal plasma cells and no myeloma related end organ damage or amyloidosis.
2. Lymphoplasmacytic lymphoma: frequently has MGUS IgM as a precursor (percentage is unknown). The differences between lymphoplasmacytic lymphoma and MGUS IgM are also clinical, not morphologic: MGUS has a lower serum M protein, a lower percentage of bone marrow lymphoplasmacytic infiltration and no associated symptoms (anemia, constitutional symptoms, hyperviscosity, lymphadenopathy or hepatosplenomegaly).
3. Chronic lymphocytic leukemia (CLL) / small lymphocytic lymphoma (SLL): virtually all CLL cases evolve from B cell monoclonal lymphocytosis; however, the differences are primarily based on the absolute cell counts, not morphology. Of note, some patients have counts that oscillate for some time between the criteria for monoclonal B cell lymphocytosis and CLL.
4. Follicular lymphoma: this common lymphoma (20 - 25% of all non Hodgkin lymphomas) rarely has a morphologic precursor of follicular neoplasia in situ. This precursor has a monoclonal proliferation of BCL2 positive B cells confined to follicle centers with preservation of the lymph node architecture but without the expansion of follicles seen in follicular lymphoma. The risk of progression to clinically significant follicular lymphoma is < 5%.
5. Mantle cell lymphoma: this relatively uncommon lymphoma (10% of all non Hodgkin lymphomas) rarely has a morphologic precursor of in situ mantle cell neoplasia. This precursor has cyclin D1 positive B cells within the mantle zone with preservation of the lymph node architecture but without expansion of the mantle zone seen in mantle zone lymphoma. The risk of progression to clinically significant mantle cell lymphoma is very low.
6. Enteropathy associated T cell lymphoma: this is a rare lymphoma (< 1% of of all non Hodgkin lymphomas) whose morphologic and clinical precursor is commonly celiac disease, which is morphologically distinct from the lymphoma. Patients with celiac disease have an increased risk of this lymphoma, particularly in the first 2 years after diagnosis but less than was claimed historically (Koskinen 2020).
We now discuss the first 3 malignancies (myeloma, lymphoplasmacytic lymphoma and CLL / SLL) and their known precursors:
1 / 2. Precursors MGUS non-IgM and MGUS IgM are benign, asymptomatic disorders having a monoclonal protein (M protein) that may progress to myeloma, lymphoplasmacytic lymphoma or other malignancies. MGUS is caused by neoplastic plasma cells, which produce excess immunoglobulins and immunoglobulin fragments, measured in the blood as M proteins (note: the M in IgM means macro because it is larger than other immunoglobulin subtypes. The M in M protein means monoclonal or myeloma).
MGUS - Immunofixation shows monoclonal IgM and kappa proteins
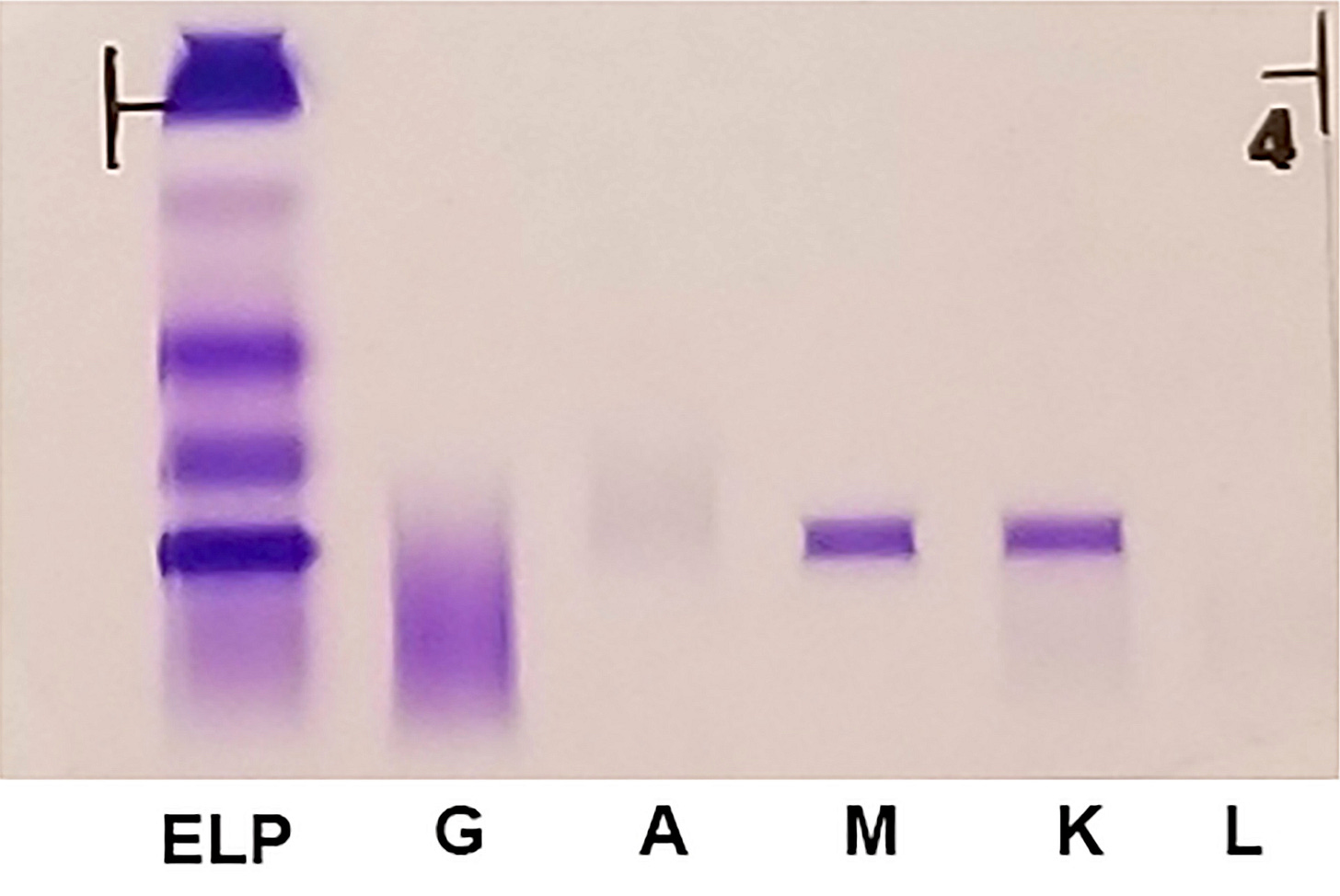
In MGUS, by definition, there is no evidence of multiple myeloma, other B cell lymphoproliferative disorders or other diseases known to produce M protein. There are 2 distinct types of MGUS: non-IgM and IgM MGUS, which are considered separate entities due to differences in cell origin, clinical features and disease progression (Campo 2022). This diagnosis is usually an incidental finding since there are no clinical symptoms.
MGUS is considered a precursor condition with an annual risk of progression of ~ 1%. MGUS may progress to multiple myeloma, amyloidosis, Waldenström macroglobulinemia (a type of lymphoplasmacytic lymphoma), solitary plasmacytoma or other lymphoproliferative disorders. The risk of progression of non-IgM MGUS is lower than for IgM MGUS (Kyle 2018).
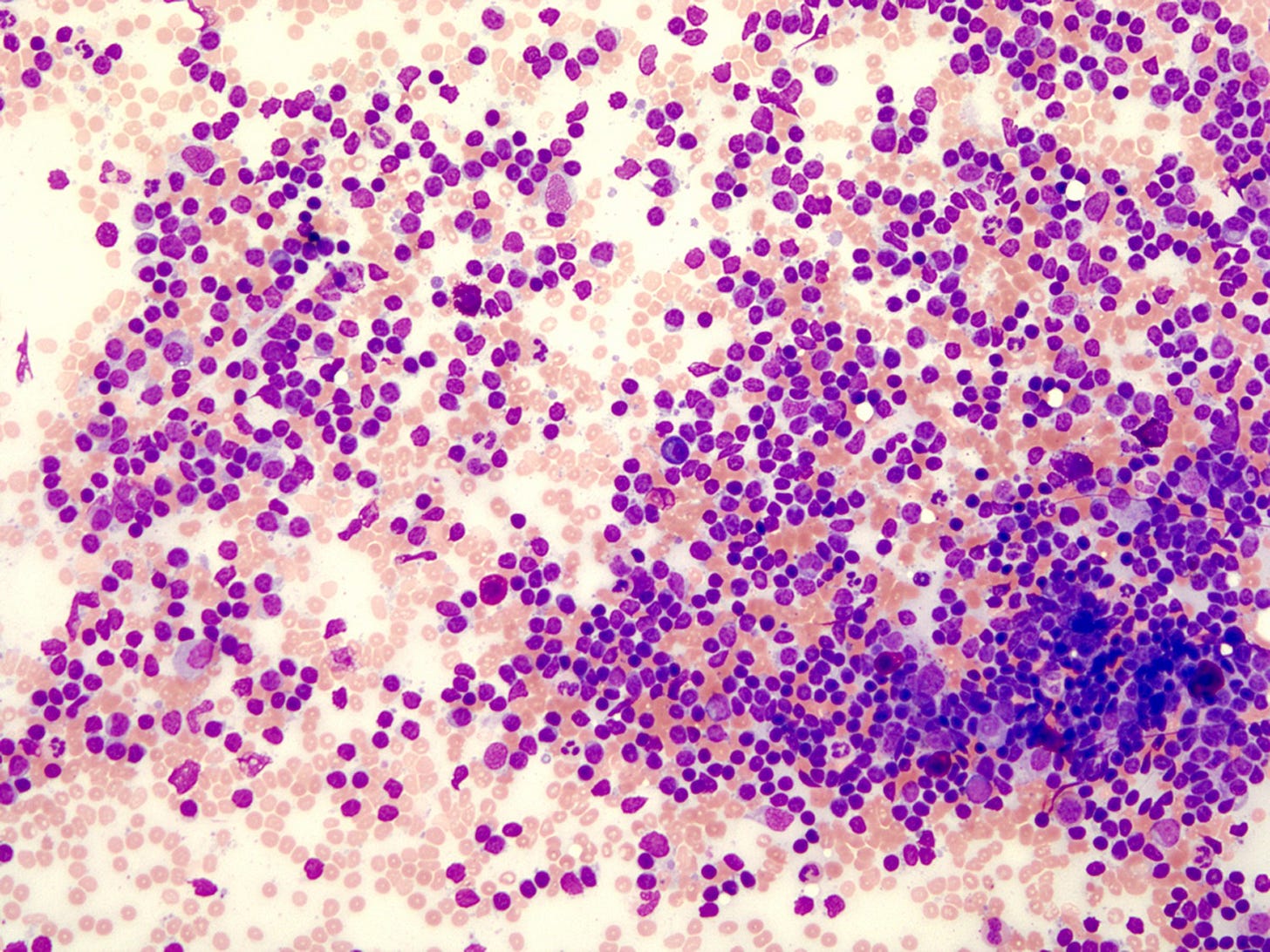
MGUS
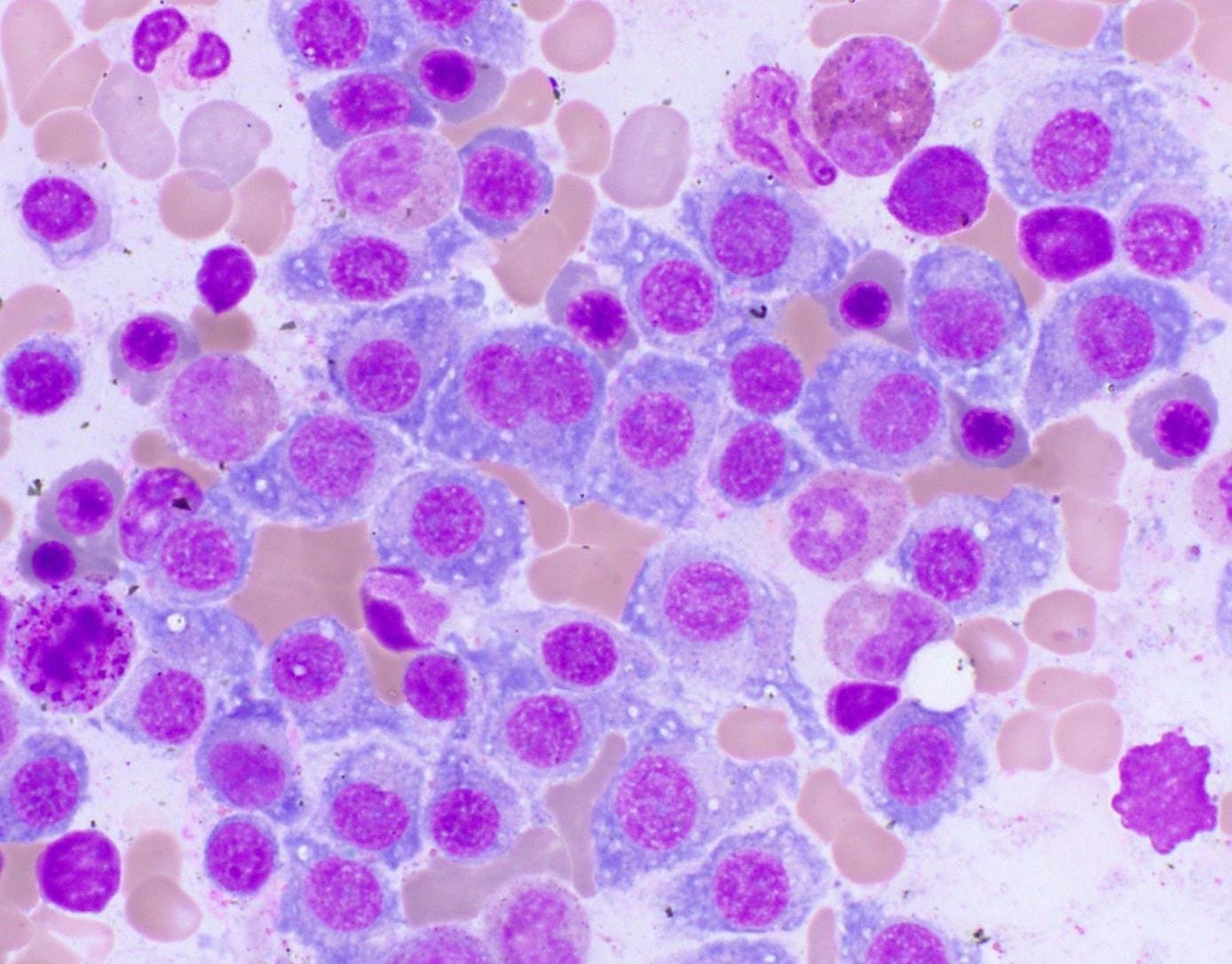
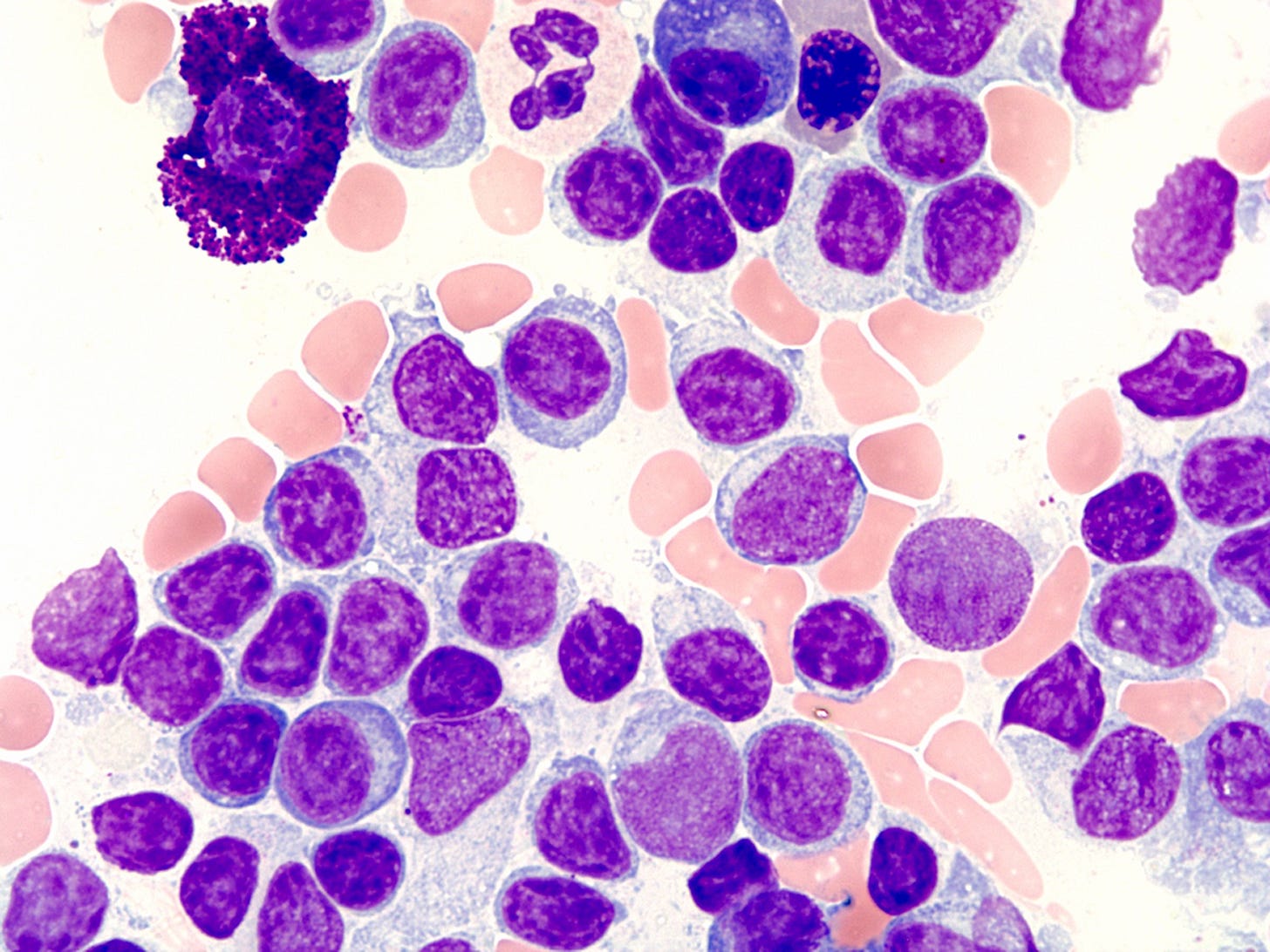
1. Plasma cell myeloma (multiple myeloma) is a bone marrow based, multifocal plasma cell malignancy usually associated with a monoclonal immunoglobulin (M protein) in serum or urine and evidence of related organ damage. Its diagnosis requires the synthesis of clinical, laboratory, radiologic and histologic findings, specifically a high serum or urine M protein, clonal plasma cells in the bone marrow and end organ damage related to the plasma cell malignancy.
The American Cancer Society estimates that in 2024 there will be 36,000 myeloma cases and 12,500 deaths in the U.S. The average lifetime risk for myeloma in the U.S. is ~ 1 in 103 for men and ~ 1 in 131 for women. The risk is higher for African American people than White people. The average age at diagnosis is 70 years. Almost all patients have prior MGUS. Other risk factors are unknown.
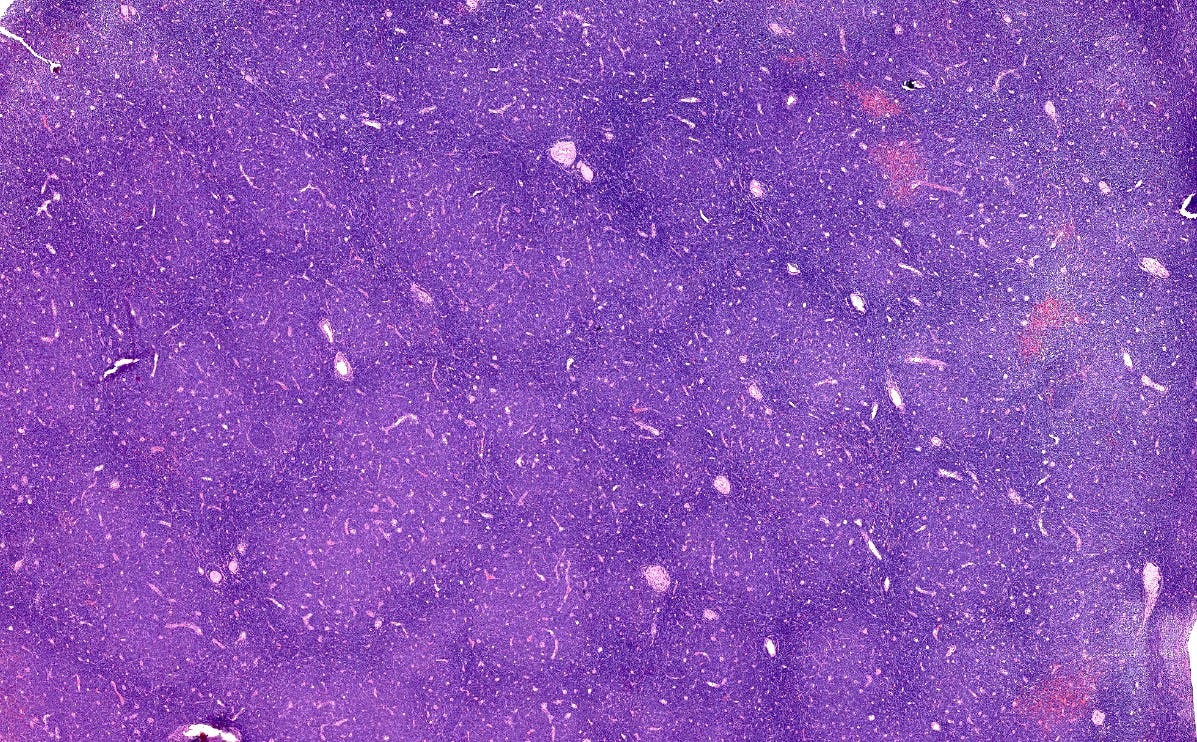
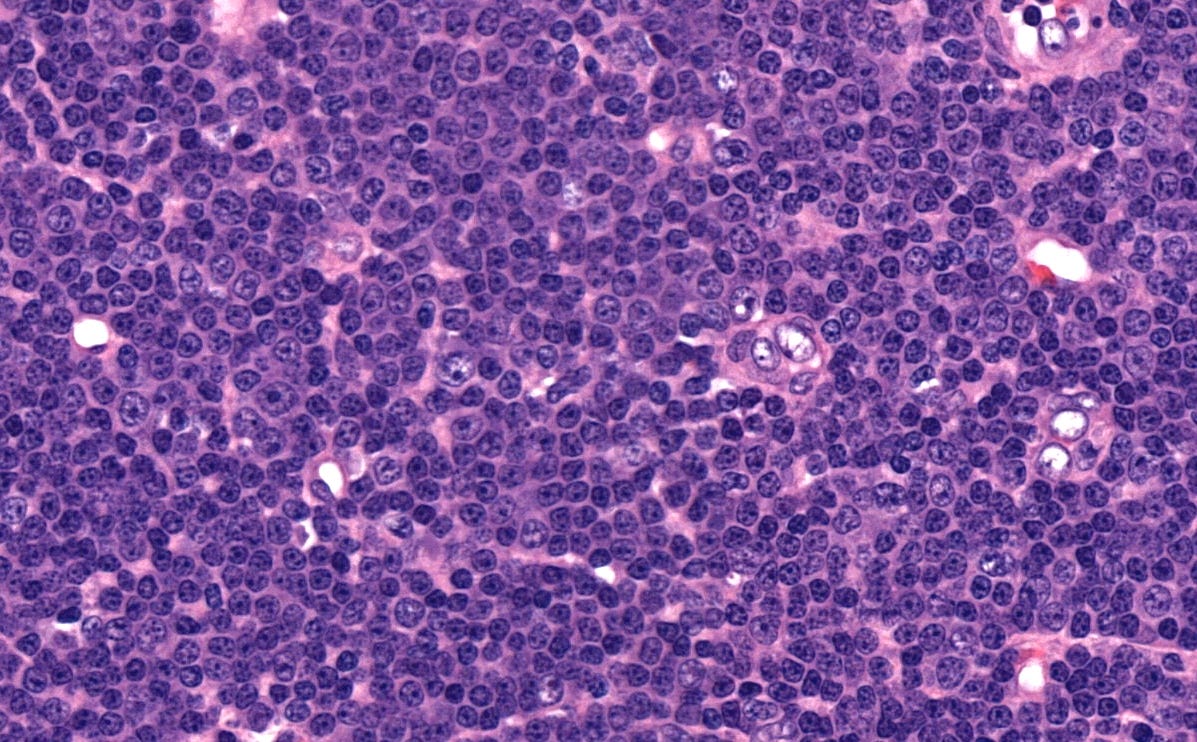
Myeloma
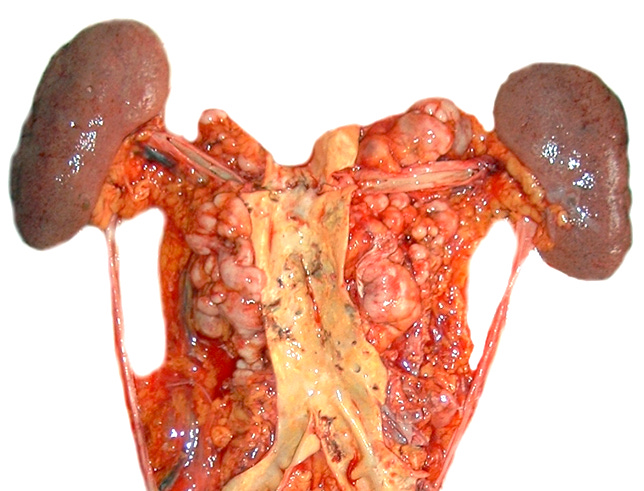
2. Lymphoplasmacytic lymphoma is a malignancy composed of small B lymphocytes, plasmacytoid lymphocytes and plasma cells. It usually involves the bone marrow, sometimes the lymph nodes and spleen. Waldenström macroglobulinemia is a subtype associated with IgM monoclonal paraprotein in the blood.
Lymphoplasmacytic lymphoma is rare, with 1,000 - 1,500 new U.S. cases per year. The average age is in the 60s. It is associated with autoimmune disorders, particularly Sjögren syndrome and autoimmune hemolytic anemia, as well as Hepatitis C, HIV infection and rickettsiosis. MGUS IgM is a known precursor, with an estimated 1.5% of cases per year progressing to lymphoplasmacytic lymphoma. The MYD88 mutation (related to immune cell activation) is found in > 90% of cases of lymphoplasmacytic lymphoma (Hunter 2014) as well as in 50% of MGUS IgM cases.
Lymphoplasmacytic lymphoma
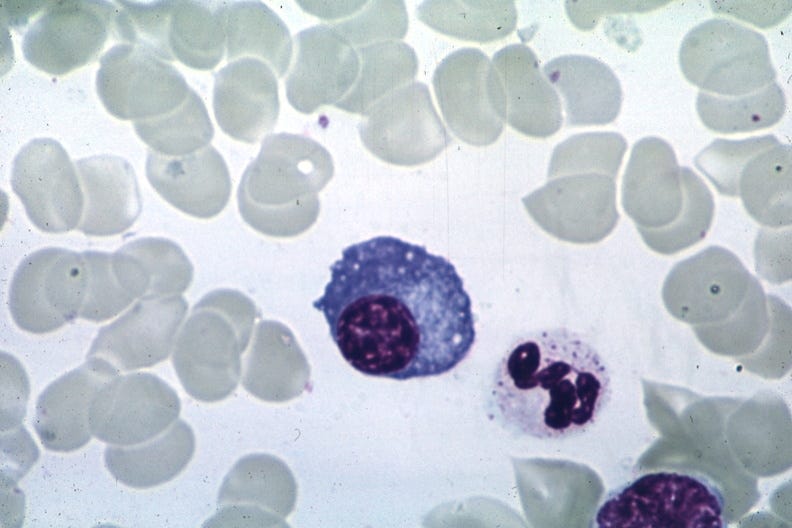
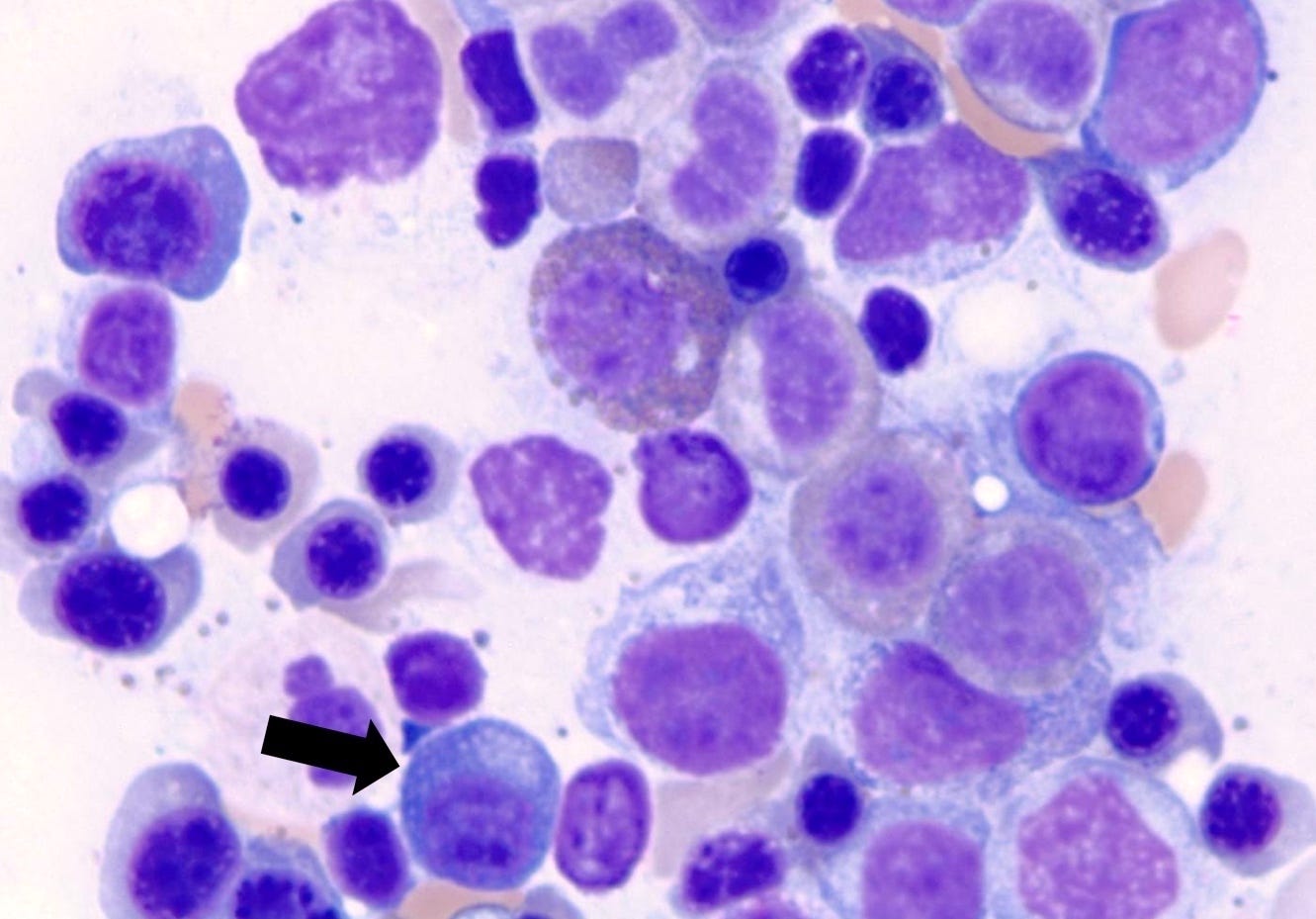
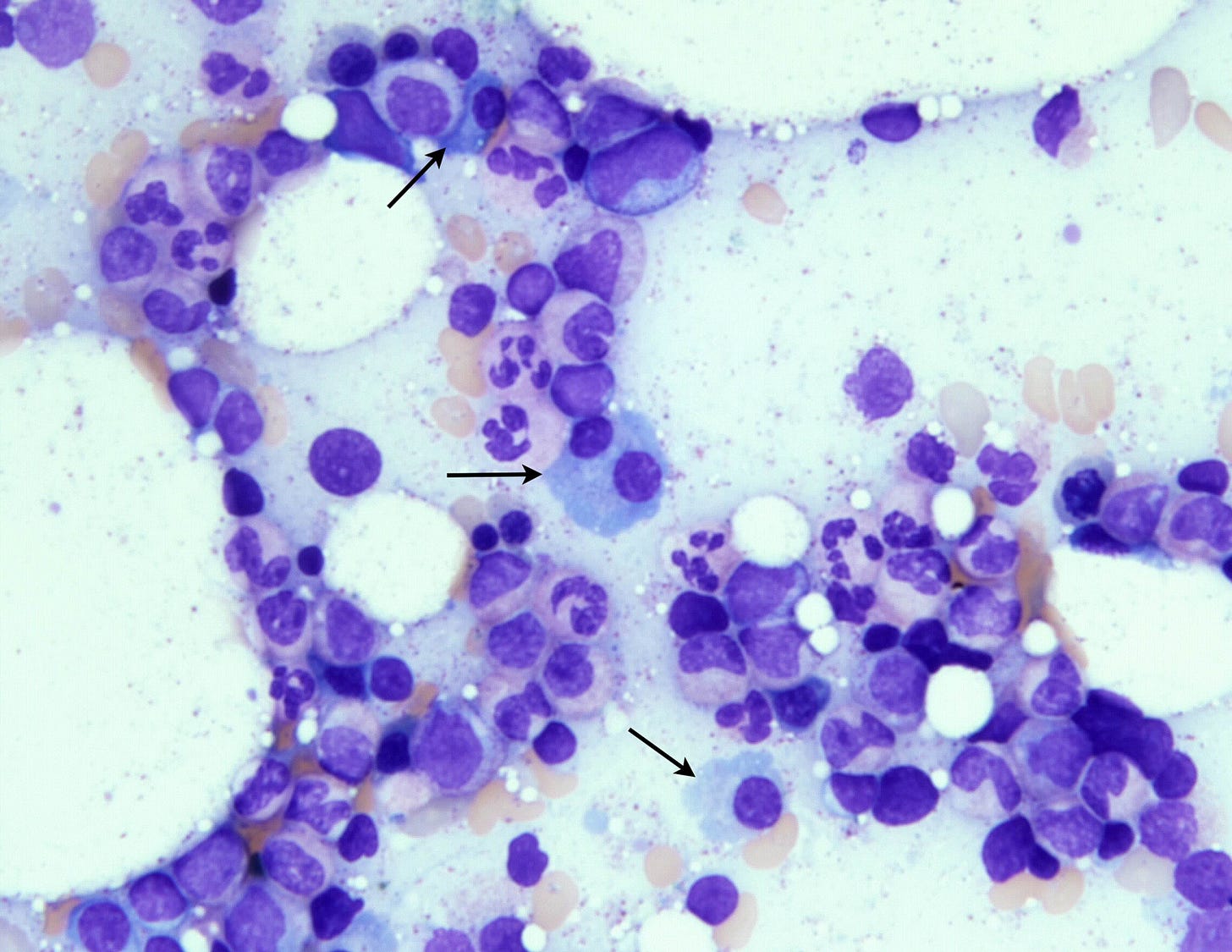
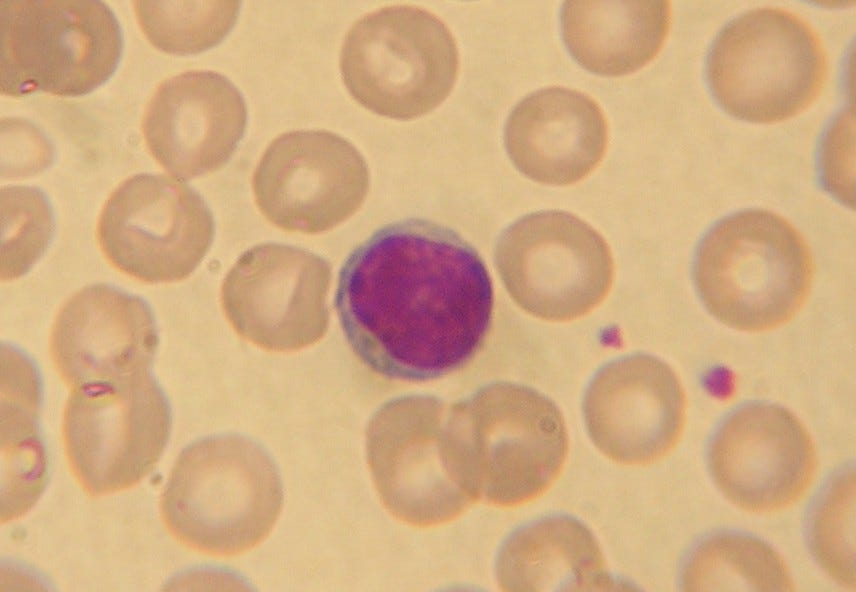
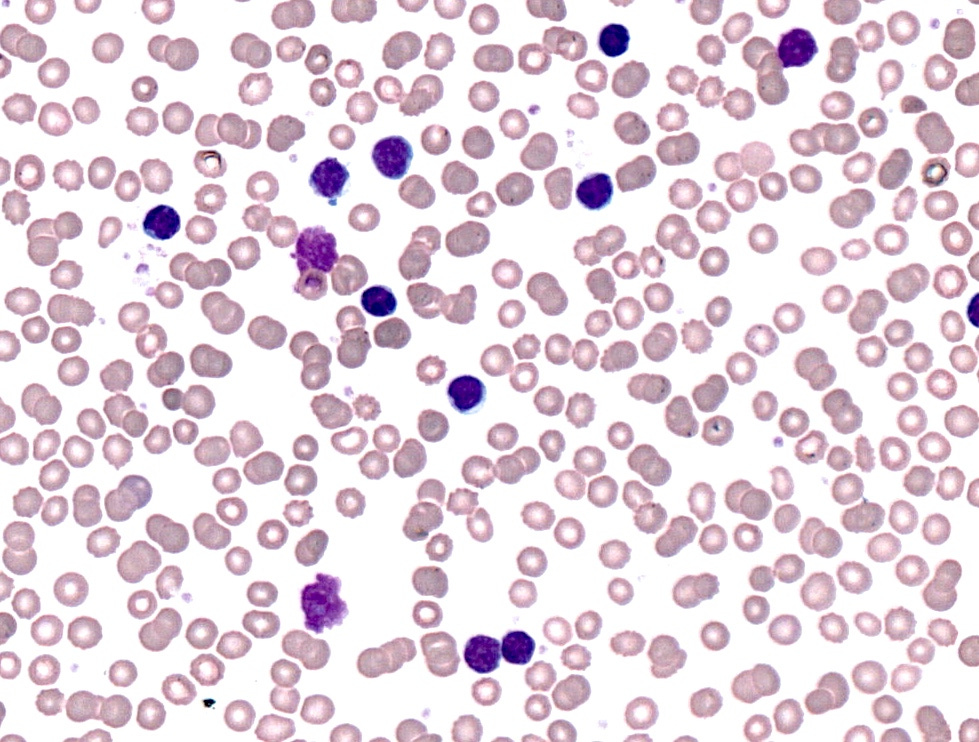
3. Precursor B cell monoclonal lymphocytosis is an asymptomatic disorder of the bone marrow and blood (but not elsewhere) with a monoclonal population of B cells in the blood of < 5 x 109/L. It occurs in < 1% of those < 40 years of age to as high as 75% of those over 90 years of age (Nieto 2009). Some cases are associated with chronic infections. Typically patients meeting this definition do NOT progress to CLL / SLL but patients with higher levels of B cells do progress at the rate of 1 - 2% per year. The B cells may have atypical features, as shown in the image below:
B cell monoclonal lymphocytosis
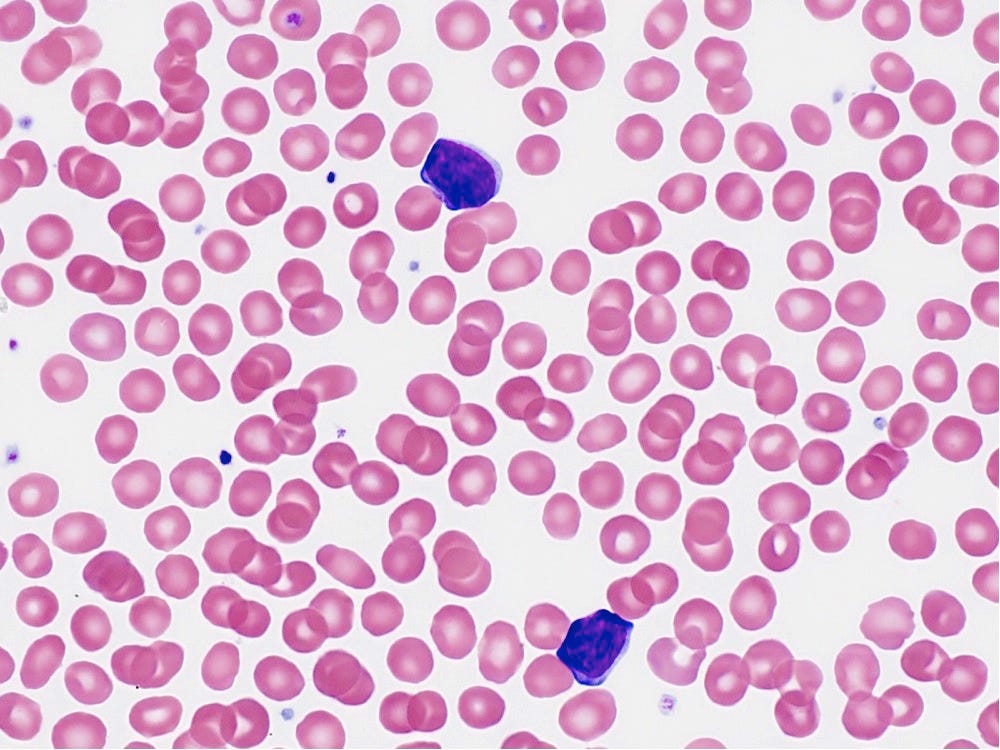
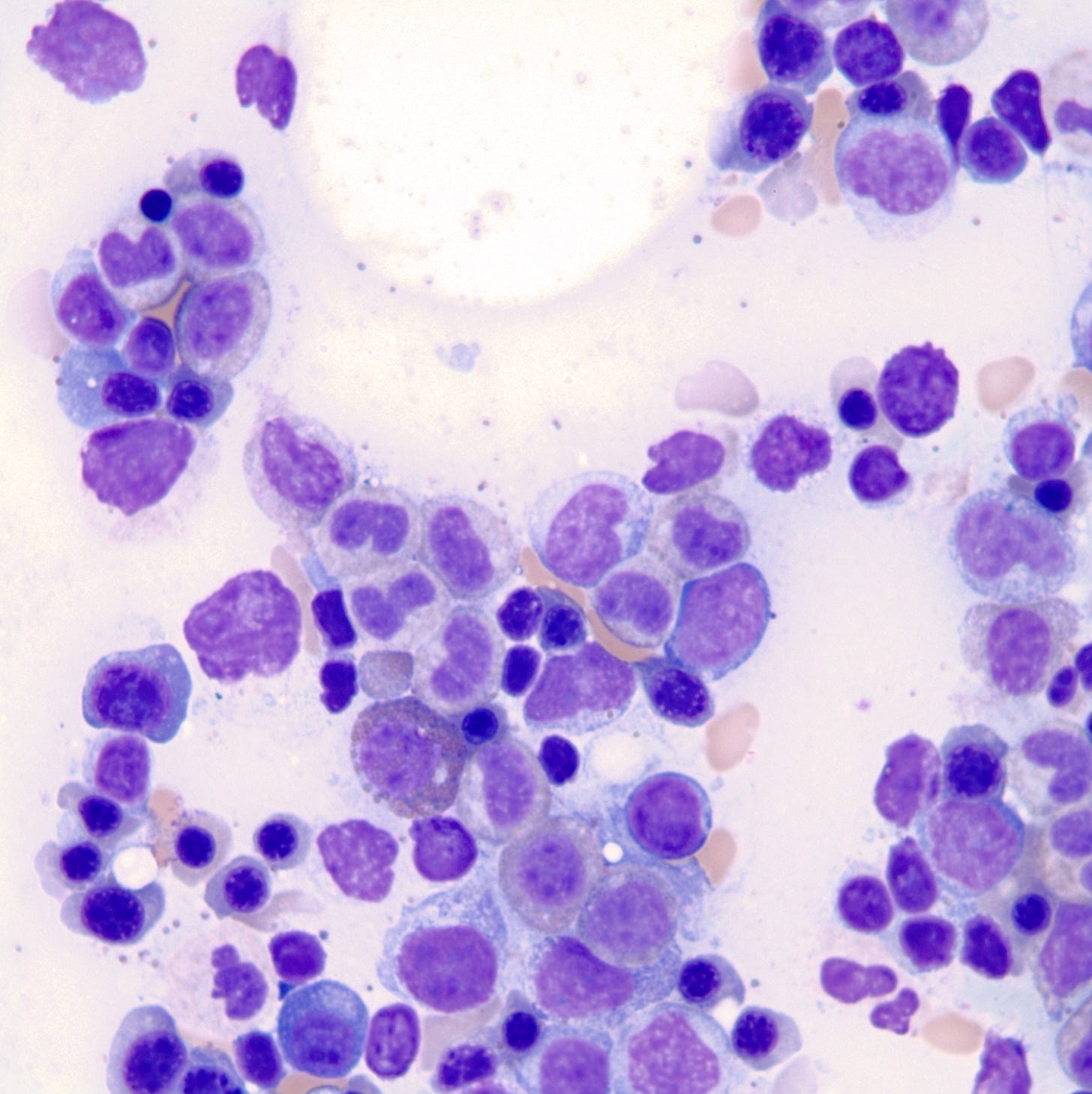
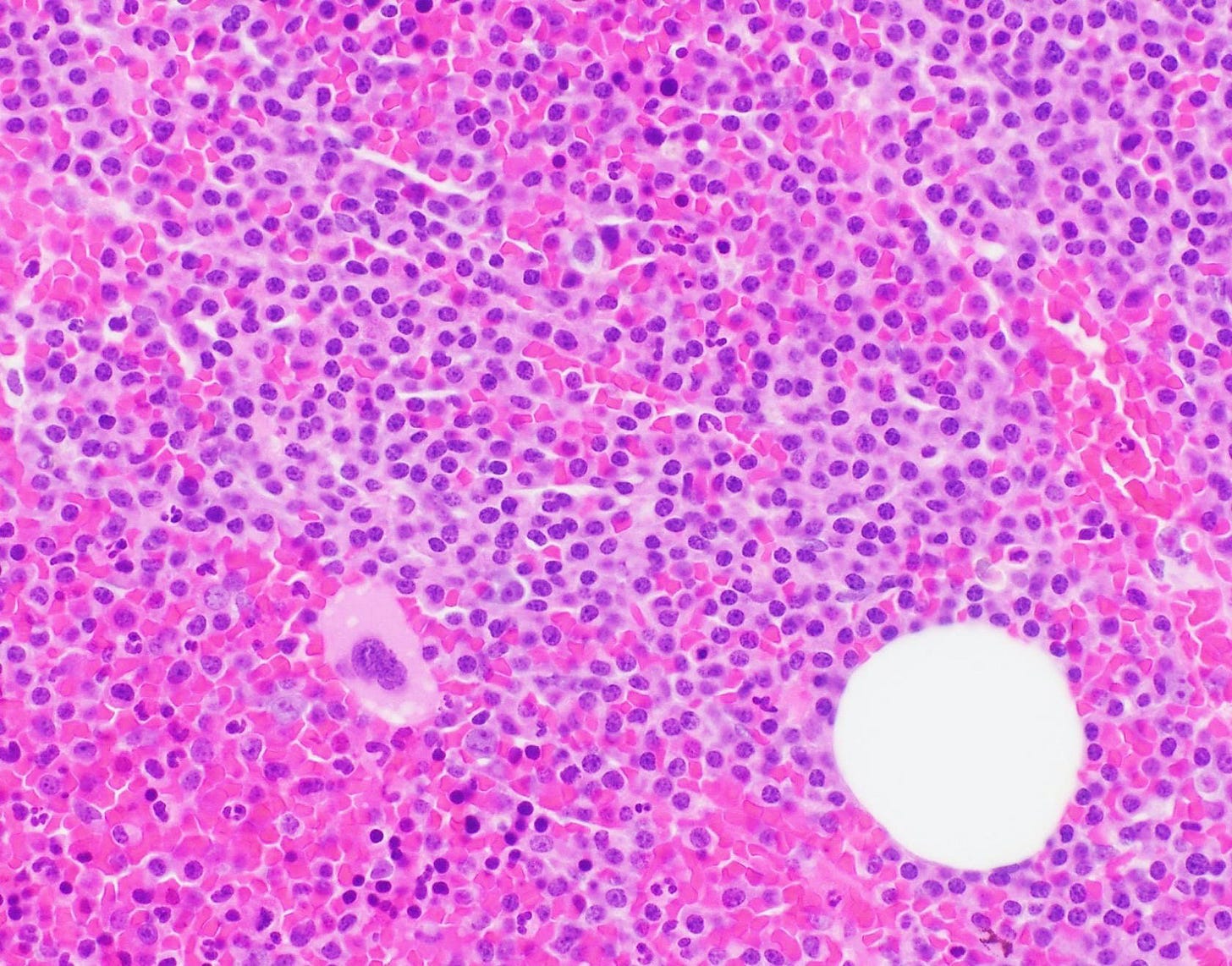
3. CLL / SLL is an indolent mature B cell lymphoma and the most common adult leukemia in the Western world. Chronic lymphocytic leukemia (CLL) is composed of mature B cells with a characteristic immunophenotype exhibiting peripheral lymphocytosis (≥ 5 x 109/L) with or without nodal or extranodal manifestation. Small lymphocytic lymphoma (SLL) is defined as < 5 x 109/L CLL-like cells in the peripheral blood but with nodal or extranodal involvement, usually with bone marrow involvement. Microscopically, there are often proliferation centers, which are ill defined, pale pseudofollicles.
CLL / SLL
In part 5b, we will discuss the remaining hematological malignancies with precursors: follicular lymphoma, mantle cell lymphoma and enteropathy associated T cell lymphoma.
If you like these essays, please subscribe or share them with others. These essays will continue to be free. Instead of requesting money, we hope you repost these essays and strive to make our world a better place and yourself a better person.
Click here for the Index to Nat’s blog on Cancer and Medicine
Follow us on Substack, LinkedIn, Threads and Instagram (npernickmich) or Tribel (@nat385440b).
Follow our Curing Cancer Network through our Curing Cancer Newsletter, on LinkedIn or Twitter or the CCN section of our PathologyOutlines.com blog. Each week we post interesting cancer related images of malignancies with diagnoses plus articles of interest. Please also read our CCN essays.
Latest versions of our cancer related documents:
Strategic plan to substantially reduce cancer deaths (June 2023)
American Code Against Cancer (how you can prevent cancer) (January 2023)
Cancer Precursor Project spreadsheet (May 2024) and General Overview (May 2024)
Email me at Nat@PathologyOutlines.com. Unfortunately, I cannot provide medical advice.
I also publish Notes at https://substack.com/note. Subscribers will automatically see my Notes.