Cancer precursor project - characteristics of premalignant precursors, part 4 (bone, joints and soft tissue malignancies)
26 May 2024
Our Cancer precursor project aims to better understand how cancer arises by compiling a regularly updated spreadsheet of all distinct human cancers (now 1,229) and their precursors (now 184).
In part 1, we discovered that the percentage of identified precursors varies widely by pathology subspecialty and we discussed precursors in subspecialties with epithelial sites (breast, head & neck, gyn, GI / liver, GU / adrenal and thoracic).
Epithelial malignancies often have risk factors associated with chronic inflammation (due to microorganisms, parasites, autoantigens, trauma, excess weight, diet, aging), DNA changes (due to germline changes, carcinogen exposure, radiation, aging), constitutive hormone production (estrogens, androgens, insulin) or immune system dysfunction (Pernick 2021). These risk factors promote changes in molecular pathways that often produce precursor lesions (intraepithelial neoplasia or dysplasia), in situ carcinoma (malignancies confined to the original site) and ultimately invasive malignancies.
In part 2, we discussed neuropathology related malignancies and their lack of precursors and concluded that contrary to current thinking, most nonepithelial malignancies, including central nervous system tumors, lack precursors. These nonepithelial malignancies often have no known risk factors and appear to arise from random processes or “bad luck” (Pernick 2022).
In parts 3a and 3b, we discussed the six skin related malignancies with known precursors: cutaneous squamous cell carcinoma (which is epithelial) and 5 types of melanoma. Melanoma derives from melanocytes, which are not epithelial but reside in a network of epithelial keratinocytes that, we believe, constrains their malignant transformation in a similar manner as epithelial cells.
We speculated that within the skin, the cell - cell connections of squamous epithelial cells and keratinocytes may force some malignancies to go through a premalignant, intraepithelial neoplasia phase by making the traditional malignant process more difficult to achieve. In addition, the basement membrane limits invasion unless additional DNA changes are present.
We speculated that some nonmelanotic skin malignancies may have a molecular precursor with distinct molecular patterns but no morphologic changes, but this has not been proven. The remaining skin malignancies may be initiated by a defining mutation in a single stem or progenitor cell that multiplies and acquires additional mutations and malignant properties over time; however, there is no premalignant intraepithelial neoplasm or other morphologic precursor during this transformation.
In the bone, joints and soft tissue, of 140 distinct malignancies, we have identified premalignant precursors in only 4 bone malignancies (chondrosarcoma grade 1, chondrosarcoma grades 2 & 3, osteosarcoma, giant cell tumor of bone) and in no soft tissue tumors. In these 4 malignancies, premalignant precursors are rare except in syndromic or genetic disorders.
1. Atypical cartilaginous tumor / chondrosarcoma grade 1 rarely has enchondroma or osteochondroma as a precursor. Tumors are more common in patients with multiple enchondromas or osteochondromas.
2. Chondrosarcoma, grades 2 & 3 rarely has enchondroma or osteochondroma as a precursor. Grade 2 & 3 chondrosarcomas appear to be distinct from grade 1 tumors but grade 2 and grade 3 tumors appear to be variations on a theme and not distinct from each other.
3. Osteosarcoma, NOS / conventional osteosarcoma rarely has Paget disease of bone as a precursor. Tumors are more common in patients with multifocal disease.
4. Giant cell tumor of bone, malignant rarely has Paget disease of bone as a precursor.
We now exclude known malignant precursors from our spreadsheet, such as low grade chondrosarcoma, a precursor of dedifferentiated chondrosarcoma and atypical lipomatous tumor / well differentiated liposarcoma, a precursor of dedifferentiated liposarcoma.
Enchondroma or osteochondroma as precursors of chondrosarcoma
Enchondroma is a benign cartilaginous tumor that arises within the medullary cavity of bone. It has no malignant features (i.e., no cytological atypia, mitoses, cortical invasion or soft tissue extension). It usually occurs in a sporadic setting and malignant transformation is rare (< 1%). It may be caused by somatic mutations in the IDH1 and IDH2 genes, found in 40% of sporadic enchondromas and also found in gliomas (brain tumors). Mutant IDH enzymes produce 2HG, which results in widespread DNA hypermethylation and may produce the enchondroma.
Patients with Ollier disease and Maffucci syndrome have multiple enchondromas and IDH1 or IDH2 mutations in 80% of cases (Pansuriya 2011). Malignant transformation to chondrosarcoma occurs in up to 46% of patients with Ollier disease and 57% of patients with Maffucci syndrome (Herget 2014). Although traditionally considered nonhereditary diseases, a recent study found germline changes in the HIF1A, VHL and IDH1 genes in some patients (Poll 2022), which we speculate might cause multiple enchondromas and malignant transformation.
Endochondroma




Osteochondroma (exostosis) is a benign bone surface tumor composed of mature bone with a cartilage cap. It may be solitary or occur as multiple hereditary exostoses. It constitutes 10% of all bone tumors and 35% of benign bone tumors, is more common in men and typically occurs in children or teenagers.
Osteochondromas, either solitary or as multiple hereditary exostoses, are associated with loss of function mutations in the EXT1 and EXT2 genes (Tanteles 2015). These genes produce proteins found in the Golgi apparatus that form a complex that modifies heparan sulfate, a protein similar to heparin, which regulates blood vessel formation and blood clotting and has a role in cancer metastases. Solitary tumors have somatic mutations (i.e., develop during life) with a 1 - 2% risk of malignant transformation. Multiple hereditary exostoses have germline mutations (i.e., develop before birth) (Wutys 1998) with a 5 - 25% risk of malignant transformation.
Osteochondroma
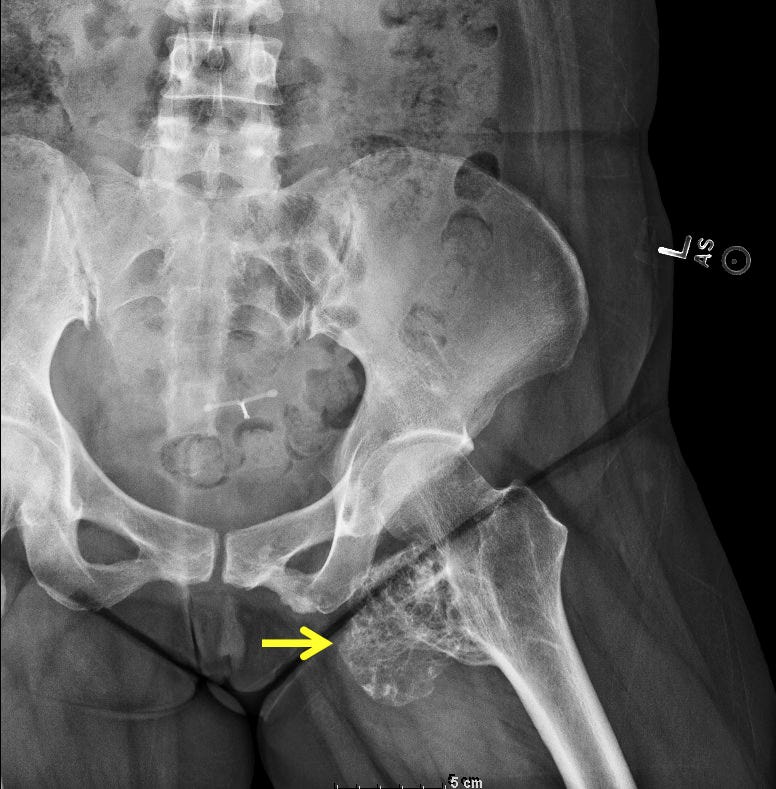



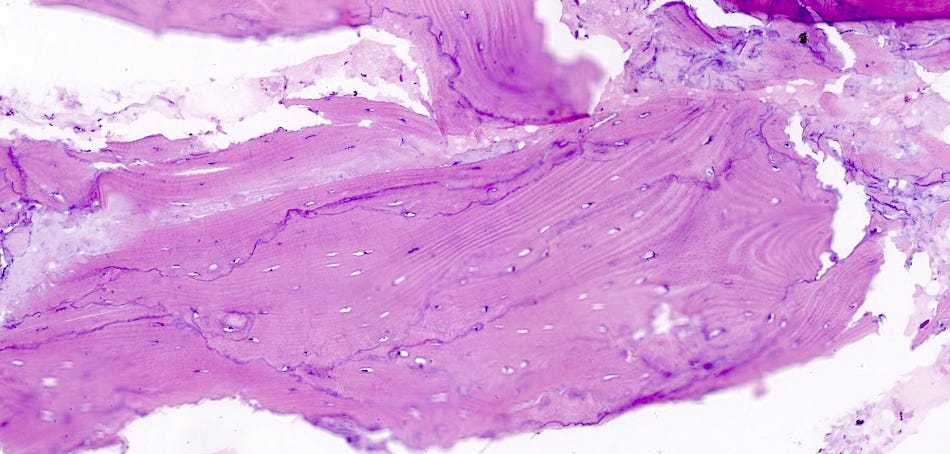
Atypical cartilaginous tumor / chondrosarcoma grade 1
Atypical cartilaginous tumor / chondrosarcoma grade 1 is a locally aggressive, hyaline cartilage producing neoplasm (abnormal growth of tissue, usually initiated by division of a single cell). Tumors in long and short tubular bones are termed atypical cartilaginous tumors but tumors in flat bones, including the pelvis, scapula and skull base are termed chondrosarcoma grade 1. These tumors have a good prognosis, with recurrence in only 10%, typically due to incomplete resection in difficult locations. They may recur as higher grade (more aggressive) chondrosarcomas. Xrays are essential for the diagnosis of this tumor because, microscopically, the tumors may appear benign.
Atypical cartilaginous tumor / chondrosarcoma grade 1






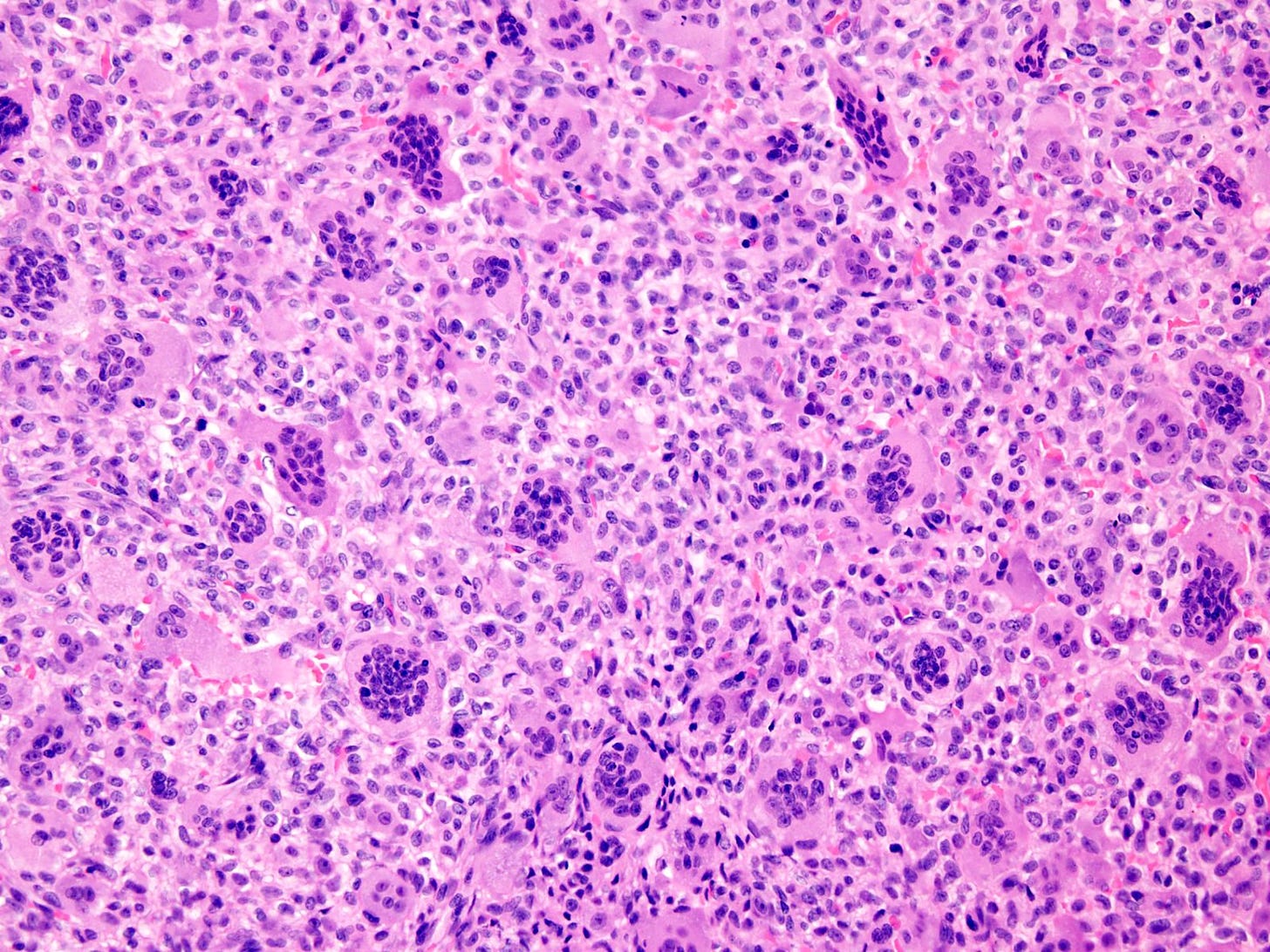
These chondrosarcomas are invasive malignancies characterized by the formation of a cartilaginous matrix. They may (secondary) or may not (primary) be associated with a preexisting enchondroma or osteochondroma. Their histologic grade (2 or 3), extracompartmental spread and local recurrence are important prognostic factors. They have a 5 year survival rate of only 50% in contrast to 85% survival for atypical cartilaginous tumor / grade 1 chondrosarcoma. Treatment is typically wide surgical resection with radiotherapy.
Chondrosarcoma grades 2 & 3

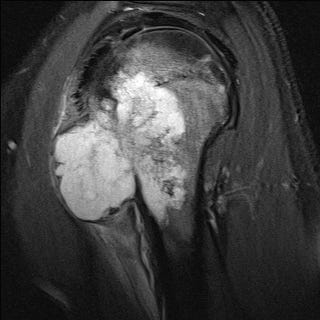



Paget disease of bone
Paget disease of bone, also called osteitis deformans, is a chronic disease of bone with accelerated bone turnover leading to disordered, poorly formed bone with increased density and an increased likelihood of fractures. It is not related to Paget disease of the breast or extramammary Paget disease, (all were discovered by Sir James Paget, a founder of pathology, Wikipedia, Al-Rashid 2015). Paget disease of bone occurs in 2% of older people and is more common in those with Western European ancestry but is rare in those with African, Scandinavian or Asian ancestry (Kravets 2018). It may be due to genetic and environmental problems that disrupt osteoclasts, including mutations in the SQSTM1 gene, which is involved in bone remodeling.
Patients with Paget disease of bone are generally asymptomatic or have mild symptoms. They often are diagnosed only after a fracture. Paget disease rarely progresses to osteosarcoma (Al-Rashid 2015) or malignant giant cell tumor of bone (Rendina 2015).
Paget disease of bone





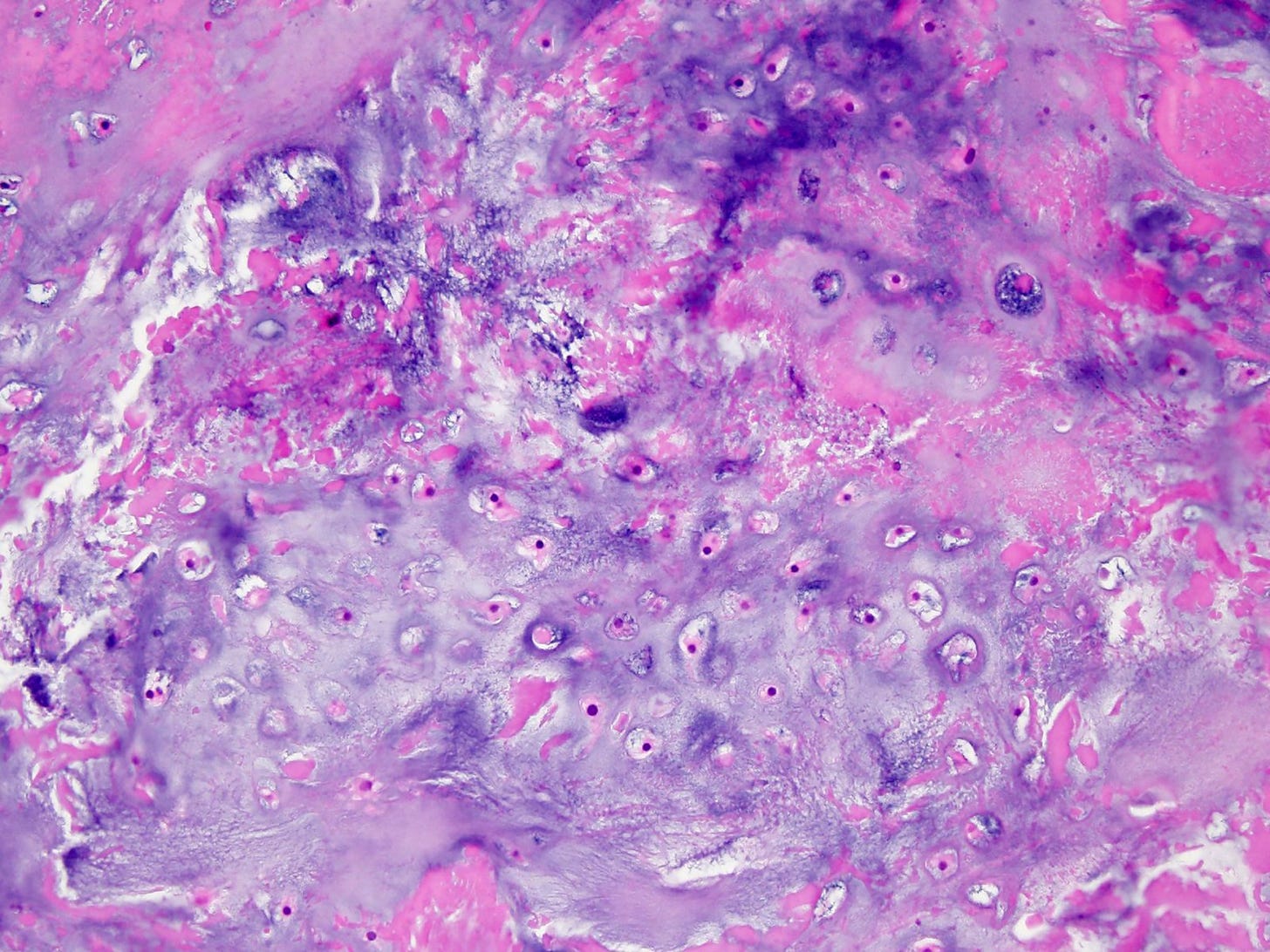
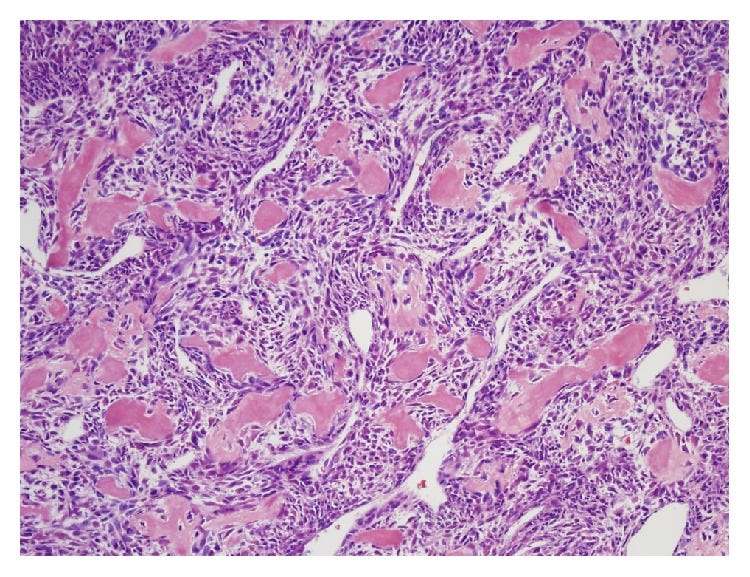
Osteosarcoma, NOS (conventional osteosarcoma) is a malignant tumor of connective tissue in which the tumor cells produce bone or osteoid. The tumor cells typically have a destructive growth pattern. There are many subtypes based on the location and microscopic features of the tumor.
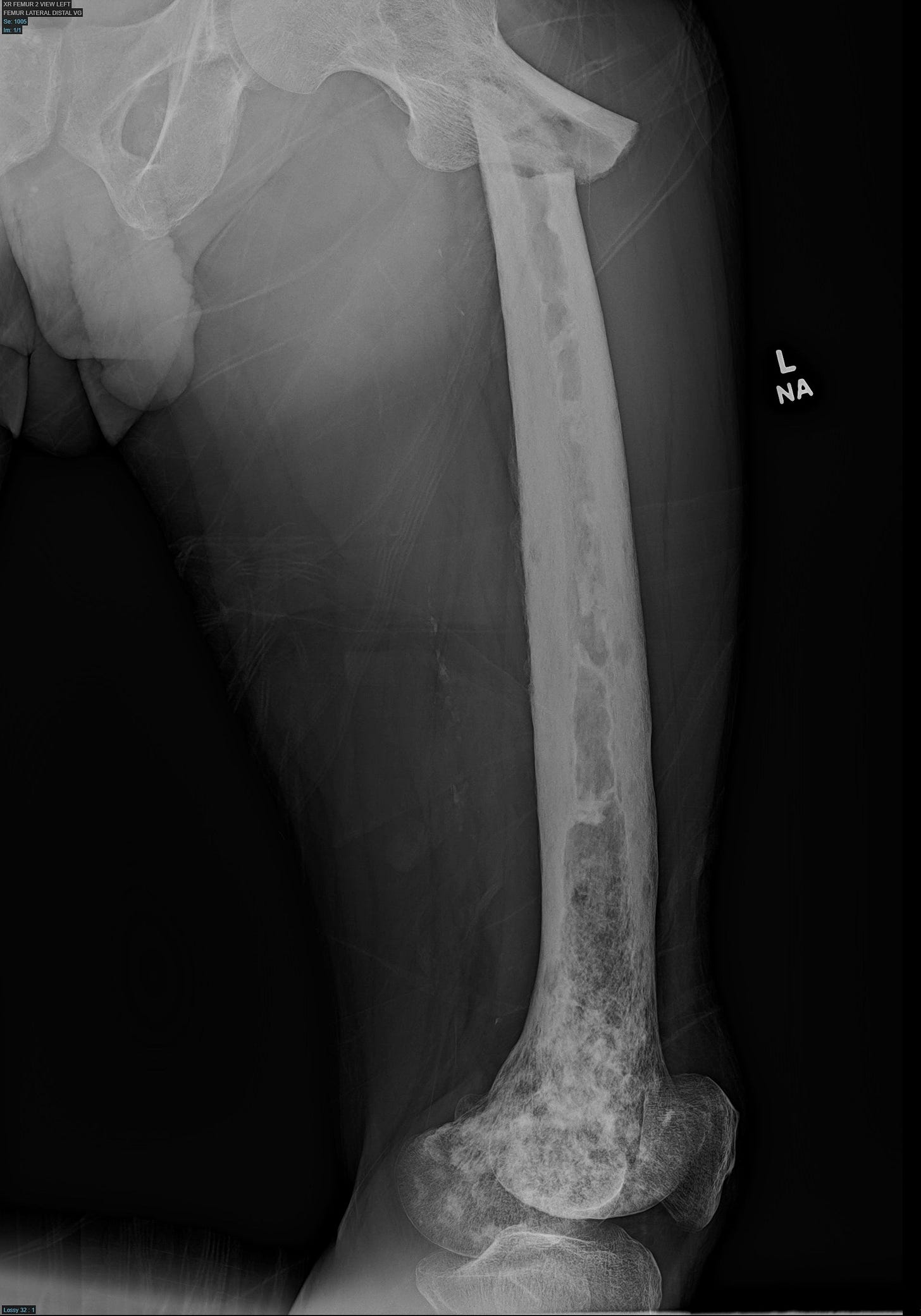
Osteosarcoma develops in about 1% of patients with sporadic Paget disease but most cases (55 - 70%) arise in patients with polyostotic disease (i.e., occurring at multiple locations, Mangham 2009). The mechanism of malignant transformation is unknown. There are no special features of osteosarcoma associated with Paget disease. The images below are of osteosarcoma in general, not associated with Paget disease.
Osteosarcoma






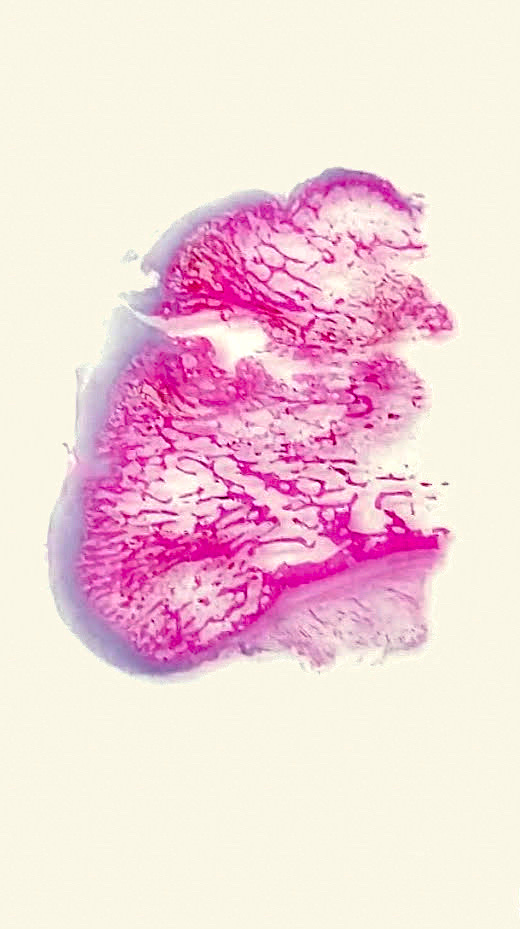
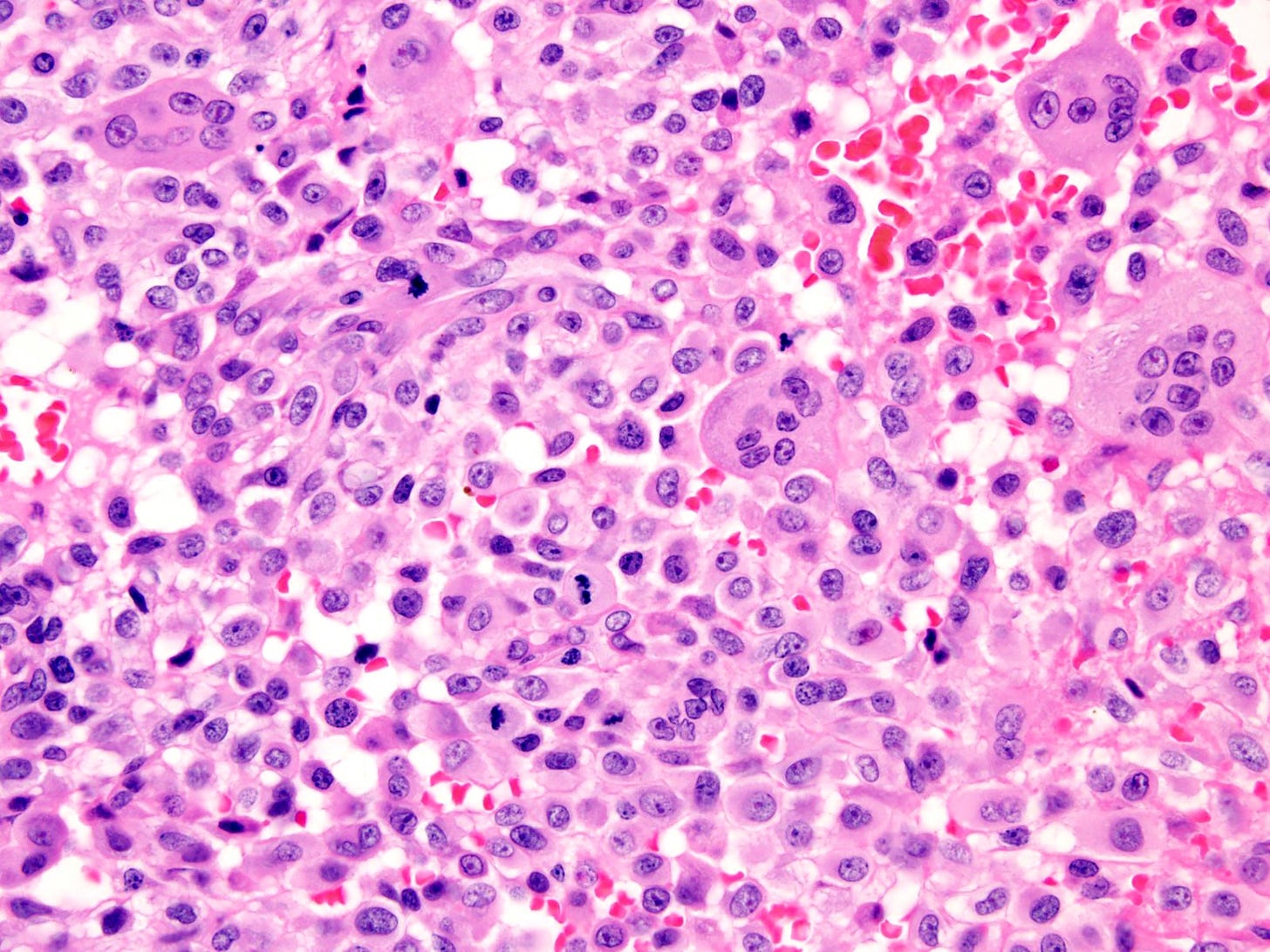
Giant cell tumor of bone is rarely associated with Paget disease of bone as a precursor. It is locally aggressive and rarely metastasizes. It is composed of neoplastic mononuclear stromal cells mixed with macrophages and osteoclast-like giant cells. Treatment is surgery or denosumab (Rutkowski 2015) with radiotherapy reserved for inoperable or refractory cases. Only rare cases are malignant, usually following radiation therapy (Palmerini 2019).
Due to the rarity of malignant giant cell tumor of bone, particularly of cases associated with Paget disease, most of the images below are of benign giant cell tumor of bone, not known to be associated with Paget disease.
Giant cell tumor of bone





Part 5 will discuss precursors associated with hematological (bone marrow and lymphoid) malignancies.
If you like these essays, please subscribe or share them with others. These essays will continue to be free. Instead of giving me money, please repost these essays and strive to make our world a better place and yourself a better person.
Click here for the Index to Nat’s blog on Cancer and Medicine
Follow us on Substack, LinkedIn, Threads and Instagram (npernickmich) and Tribel (@nat385440b).
Follow our Curing Cancer Network through our Curing Cancer Newsletter, on LinkedIn or Twitter or the CCN section of our PathologyOutlines.com blog. Each week we post interesting cancer related images of malignancies with diagnoses plus articles of interest. Please also read our CCN essays.
Latest versions of our cancer related documents:
American Code Against Cancer (how you can prevent cancer)
Email me at Nat@PathologyOutlines.com. Unfortunately, I cannot provide medical advice.
I also publish Notes at https://substack.com/note. Subscribers will automatically see my Notes.




