Cancer precursor project - characteristics of premalignant precursors, part 3b (dermatopathology)
13 May 2024, revised 17 May 2024
Our Cancer precursor project is intended to better understand how cancer arises by compiling a regularly updated spreadsheet of all distinct human cancers (now 1,230) and their precursors (now 185).
In the skin, of the 79 distinctive malignancies identified to date, we have identified only 6 malignancies associated with precursors (5 melanocytic, 1 nonmelanocytic):
Invasive melanoma: may have dysplastic nevus as precursor
Superficial spreading melanoma (low CSD [cumulative sun damage] melanoma): may have dysplastic nevus as precursor
Lentigo maligna melanoma: may have lentigo maligna as precursor
Acral melanoma: may have acral lentiginous melanoma in situ and acral nevus as precursors
Melanoma arising in giant congenital nevus: precursor is giant congenital nevus
Squamous cell carcinoma: may have actinic keratosis / keratinocytic dysplasia and squamous cell carcinoma in situ as precursors
In part 3a, we discussed the precursors of the first 3 malignancies. In part 3b, we discuss the precursors of the last 3 malignancies.
4. Acral lentiginous melanoma in situ and acral nevus are precursors of acral melanoma although both precursors are uncommon. Acral means the highest or topmost portion of the limbs (i.e., the palms, soles or under fingernails or toenails).
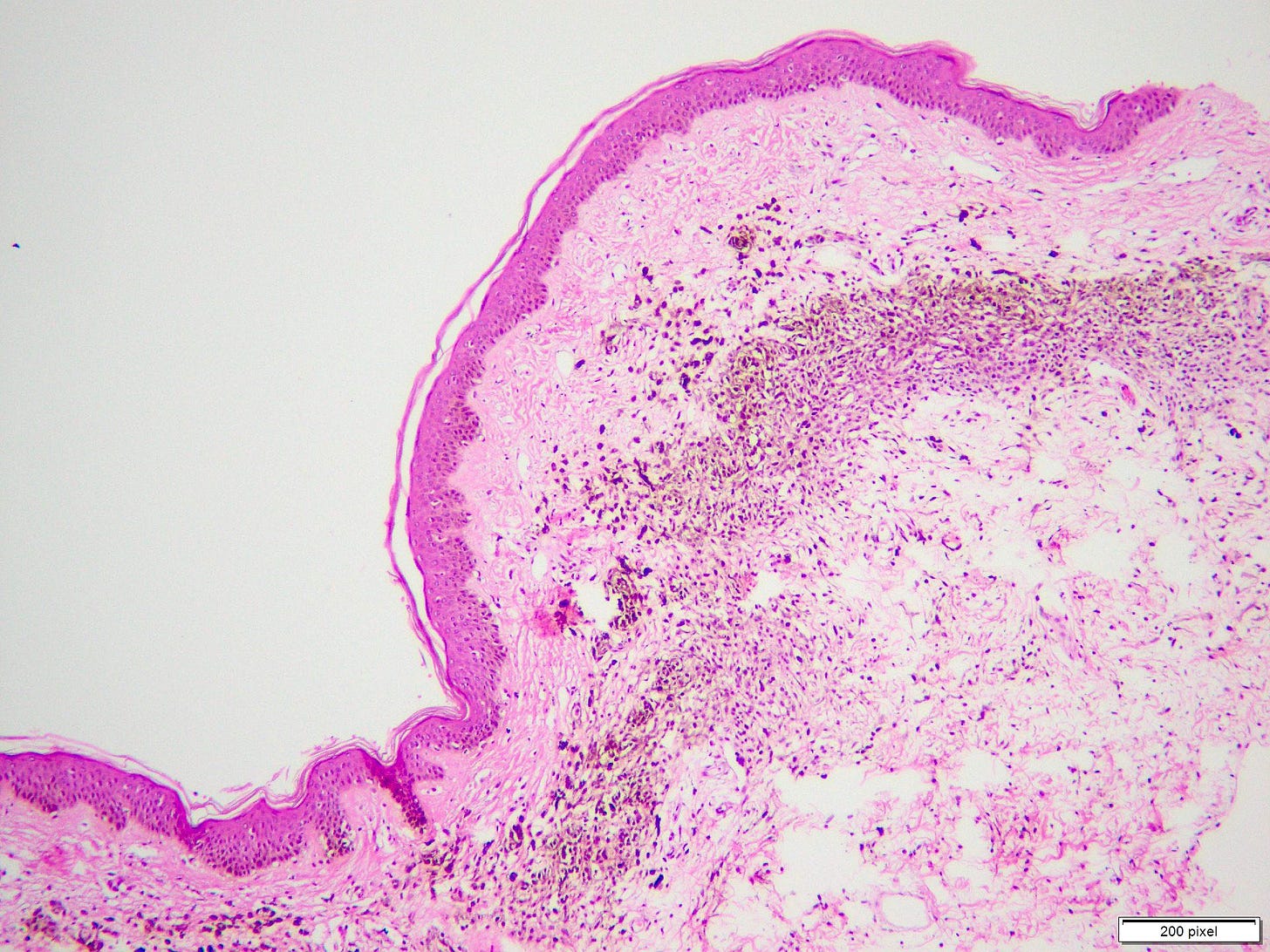
Acral lentiginous melanoma in situ

Acral nevus


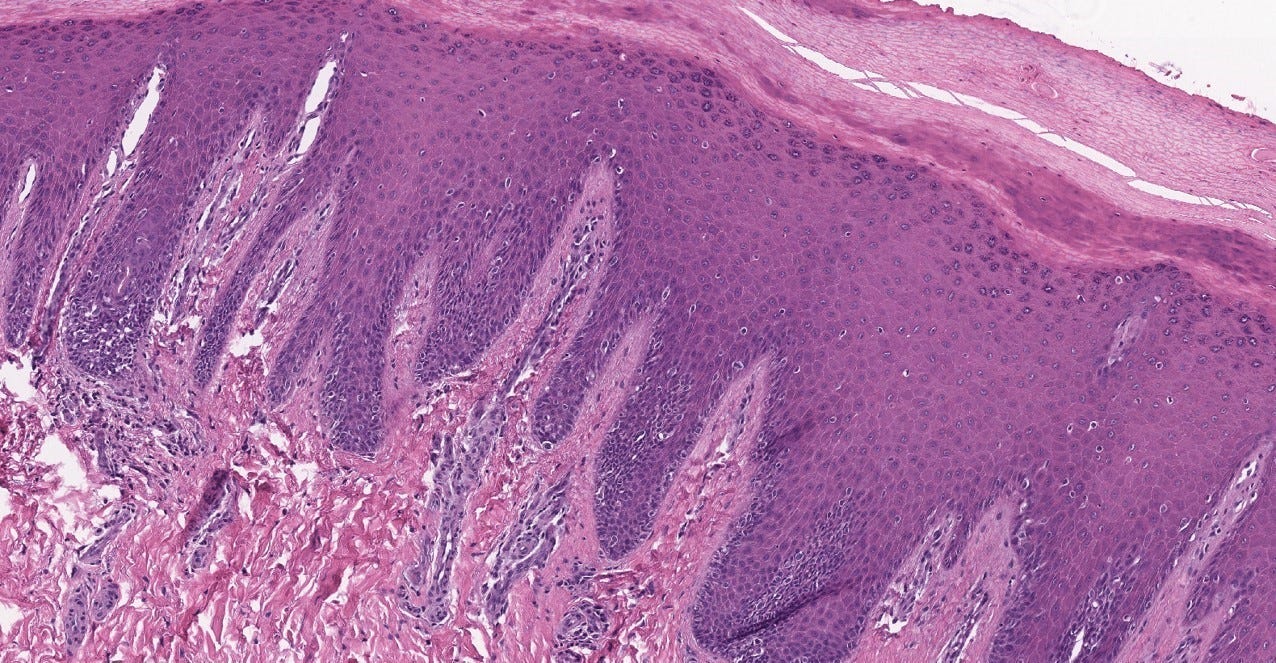
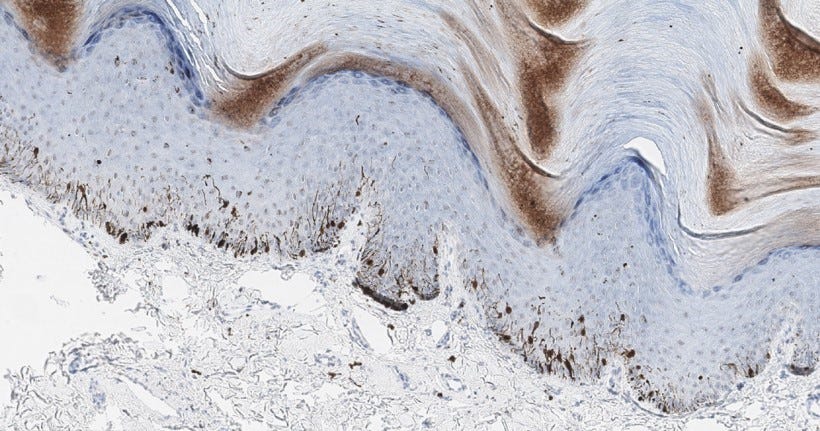
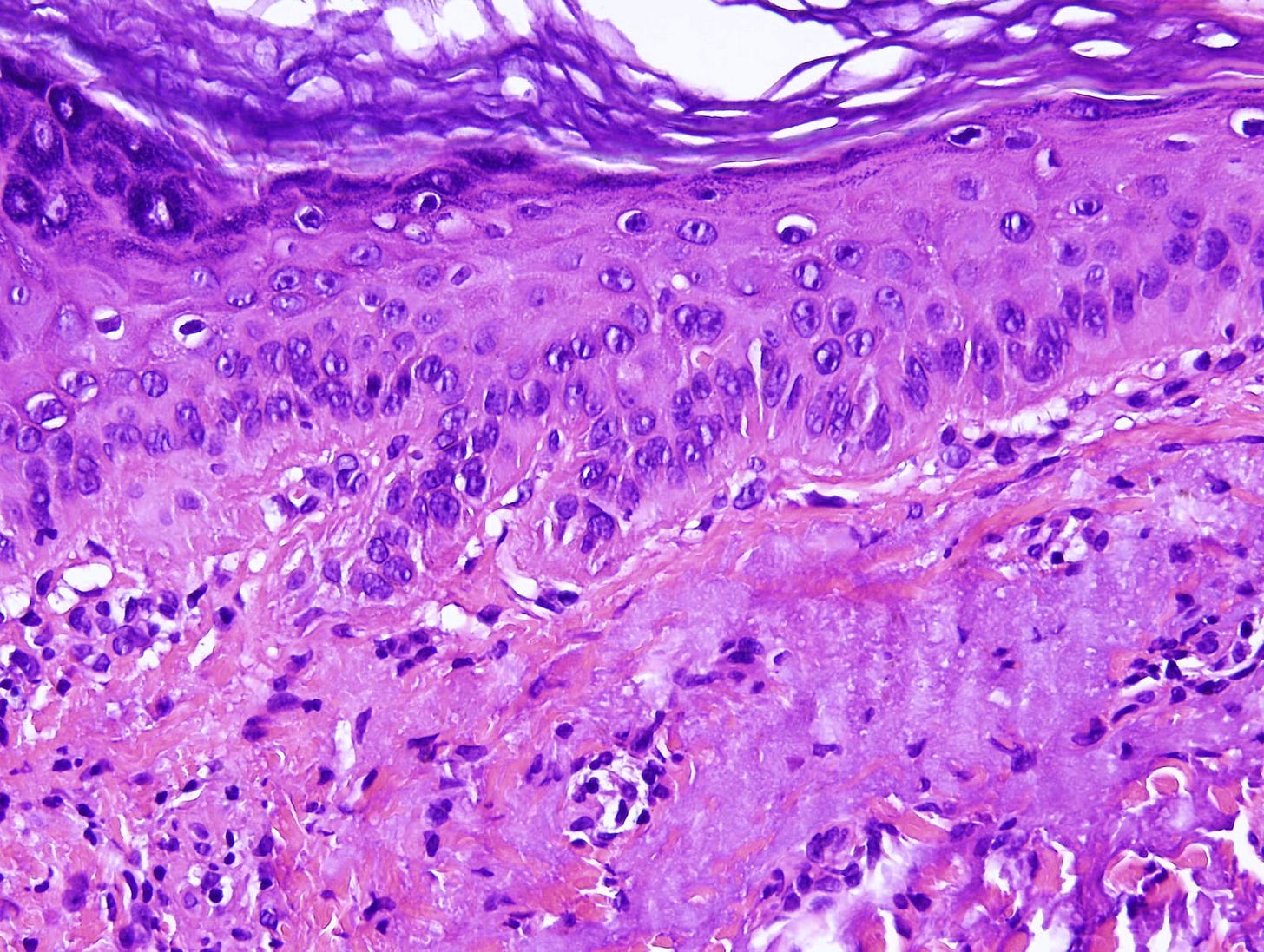
Acral lentiginous melanoma in situ demonstrates an increased number of irregularly distributed melanocytes at the base of the epidermis. These melanocytes have hyperchromatic (dark) nuclei with variable cytologic atypia. This lesion may be mistaken for melanosis, the proliferation of melanocytes with no malignant potential (Bae 2009).
Acral lentiginous melanoma

Acral melanoma is the most common type of melanoma in patients of Asian, Hispanic and African descent. Patients have an average age of onset of 63 years. Acral melanoma is rare but typically occurs in the palms, soles, digits and nail apparatus. It is associated with traumatic events, physical stress, farmers and fisherman (Lee 2021) but unlike other melanomas, family history and ultraviolet light exposure are minimal risk factors.
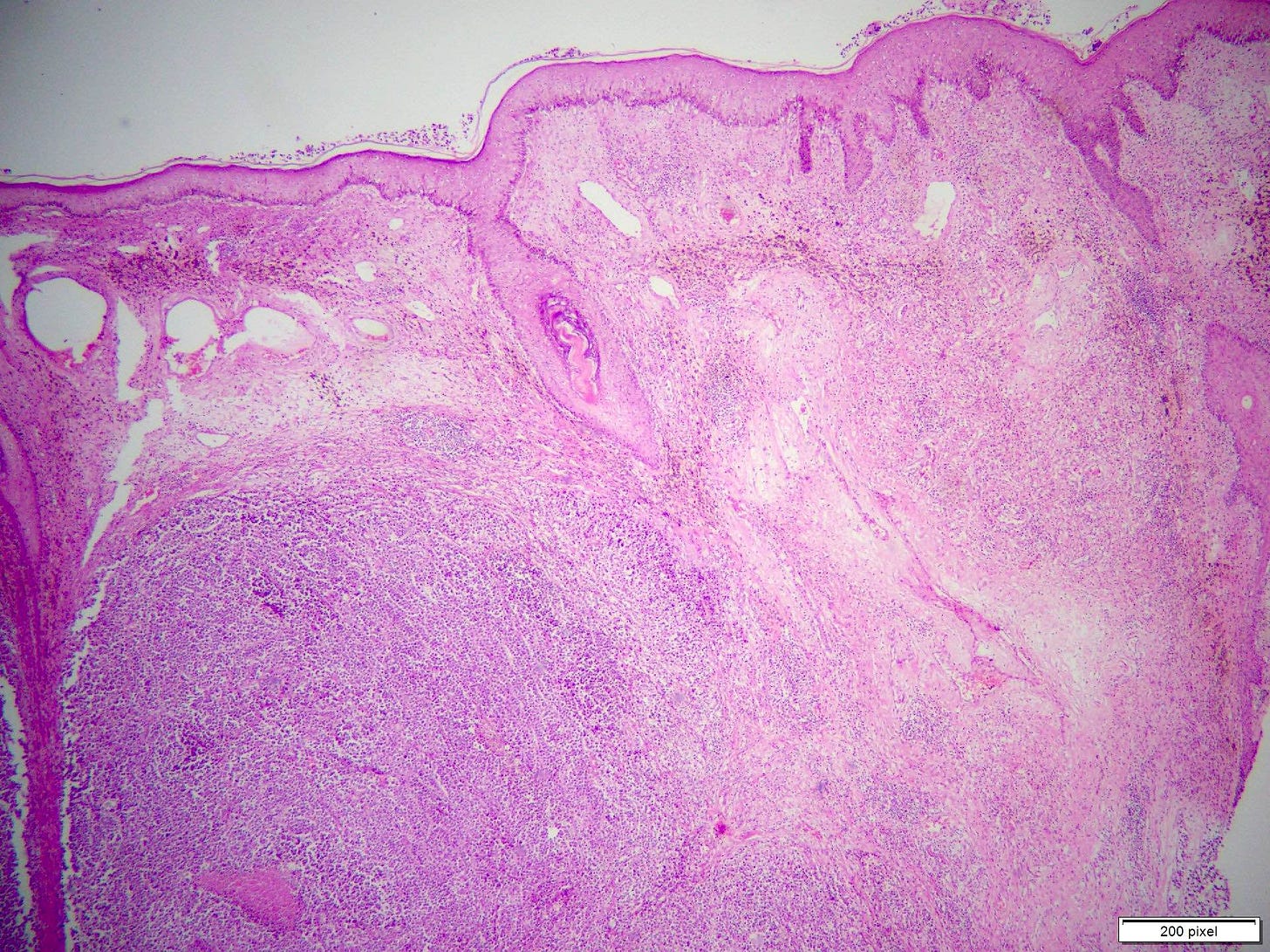
5. Giant congenital nevus is a precursor of melanoma arising in giant congenital nevus.
Giant congenital nevus

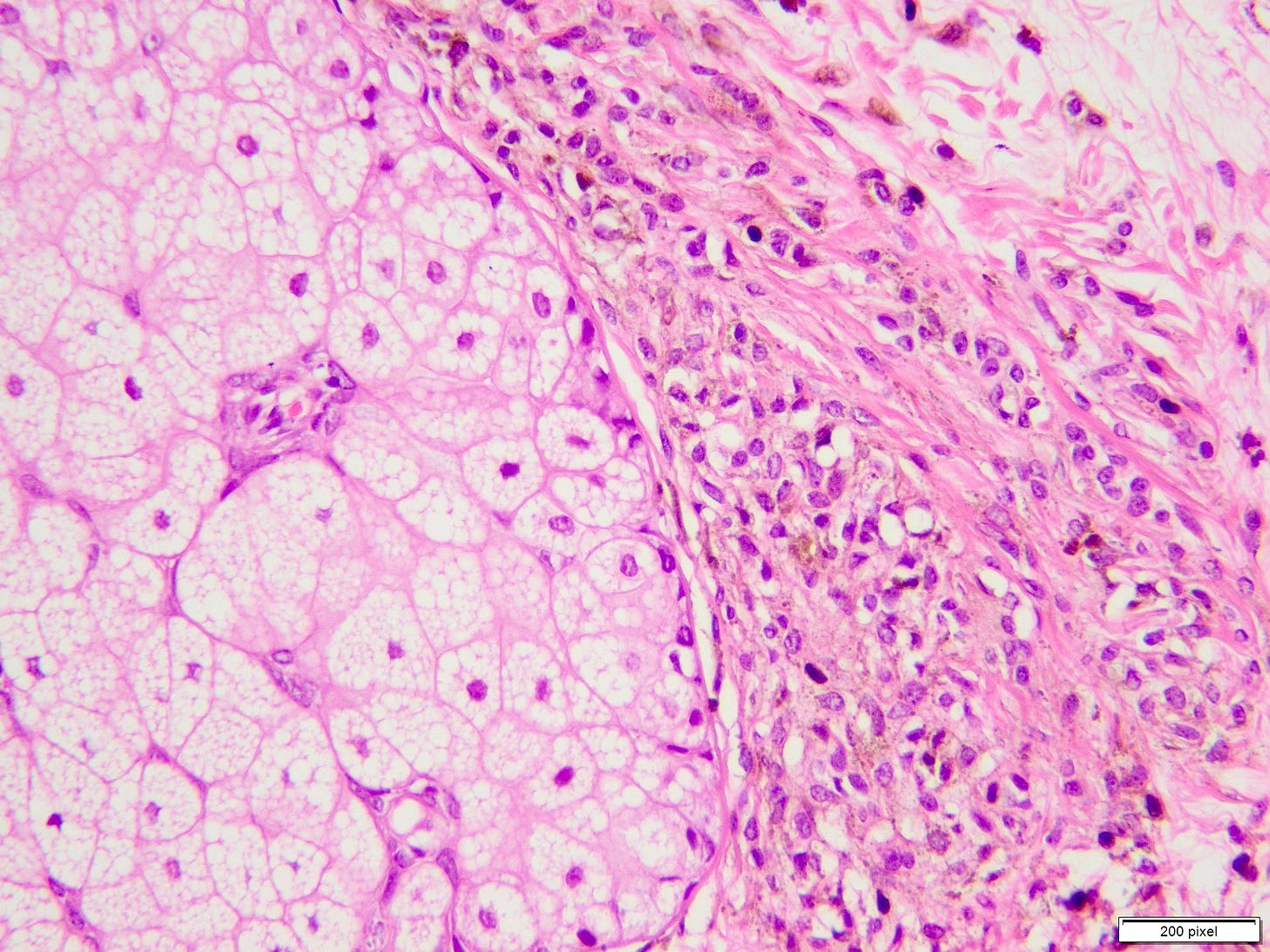
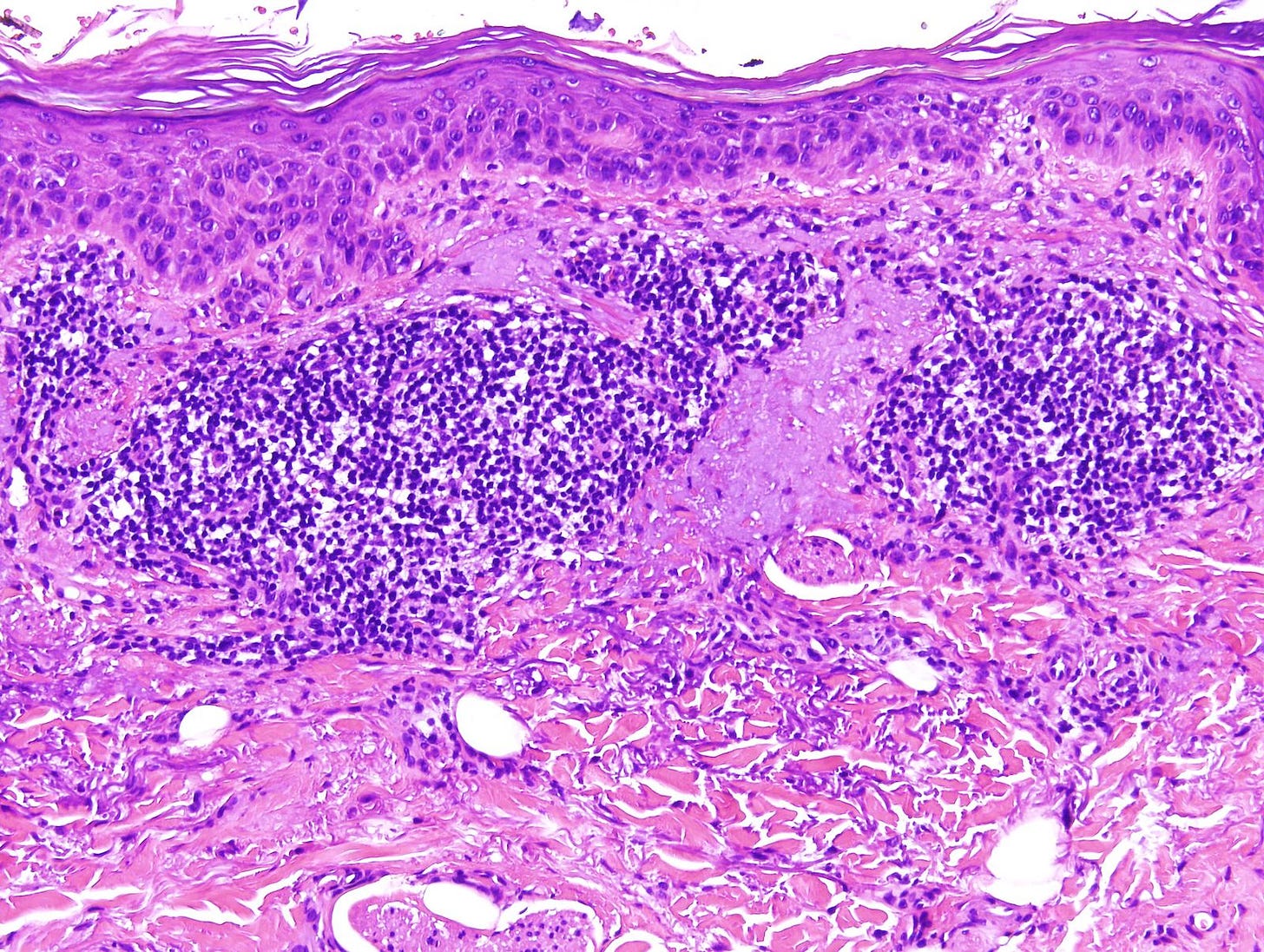
Congenital nevi are present at birth or arise within the first few postnatal weeks. Giant congenital nevi are > 40 cm in size. The risk of melanoma is directly proportional to their size.
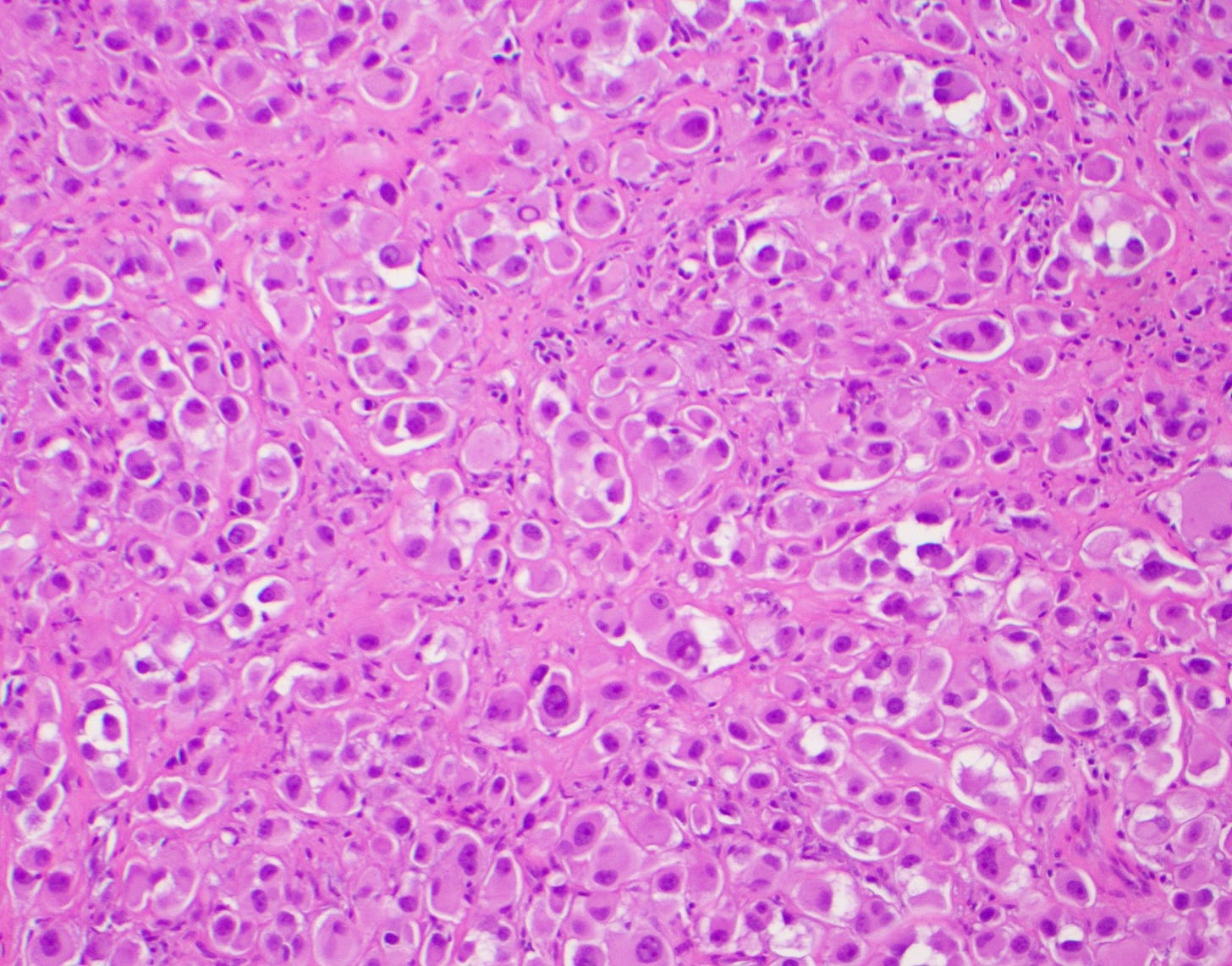
Melanoma arising in a giant congenital nevus

6. Actinic keratosis / keratinocytic dysplasia and squamous cell carcinoma in situ are both precursors of squamous cell carcinoma (SCC) in the skin.
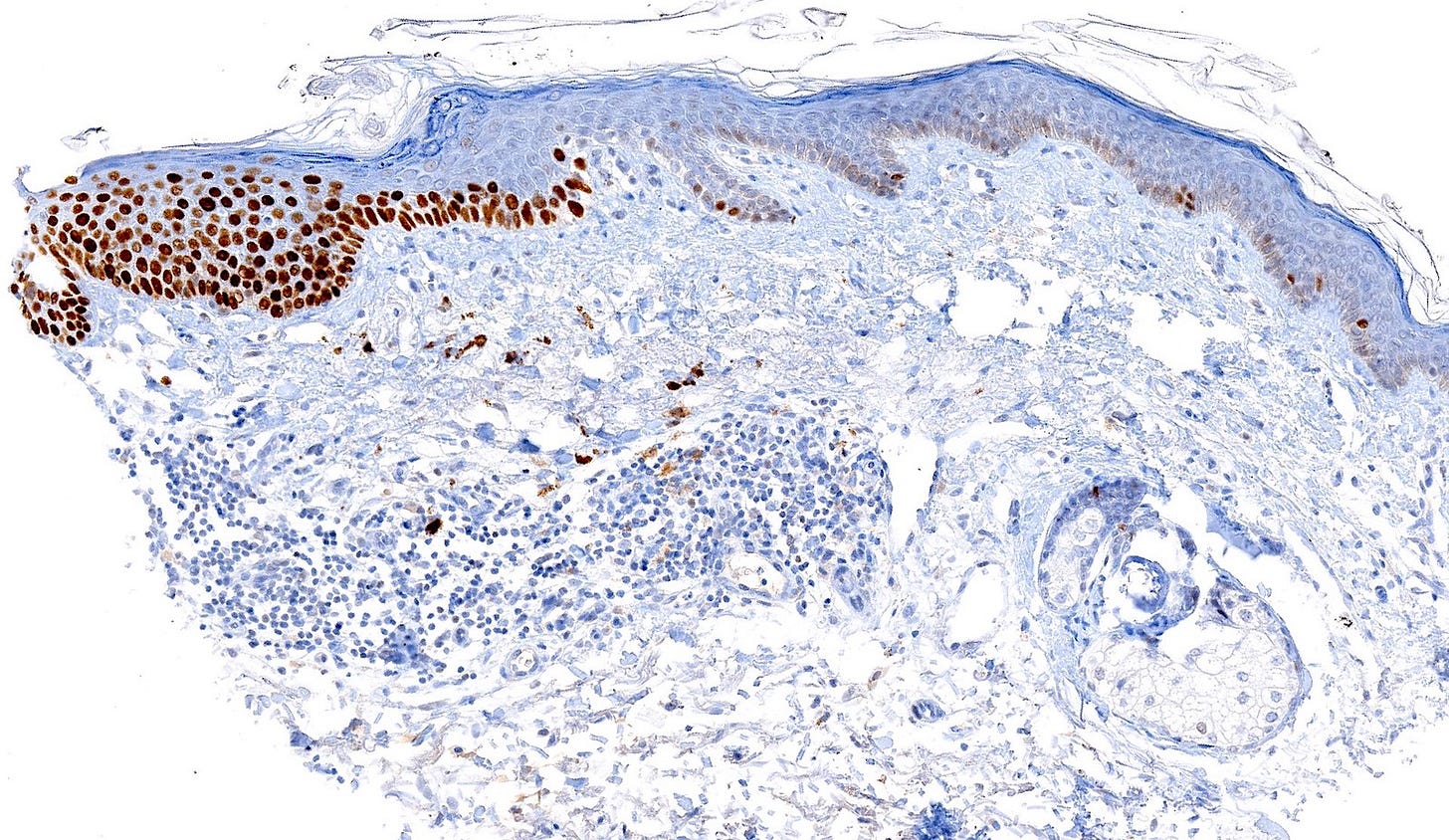
Actinic keratosis is an intraepidermal keratinocytic lesion caused by solar damage. It is the most common precursor of cutaneous squamous cell carcinoma. Typically it remains stable for long periods or regresses but in 1% of cases, it transforms into squamous cell carcinoma either by (a) atypical basal keratinocytes invading the mid to upper epidermis and transforming into invasive SCC or (b) actinic keratosis transforming directly into invasive SCC with dysplasia limited to the basal layer (Saenz-Sardà 2018).
Actinic keratosis

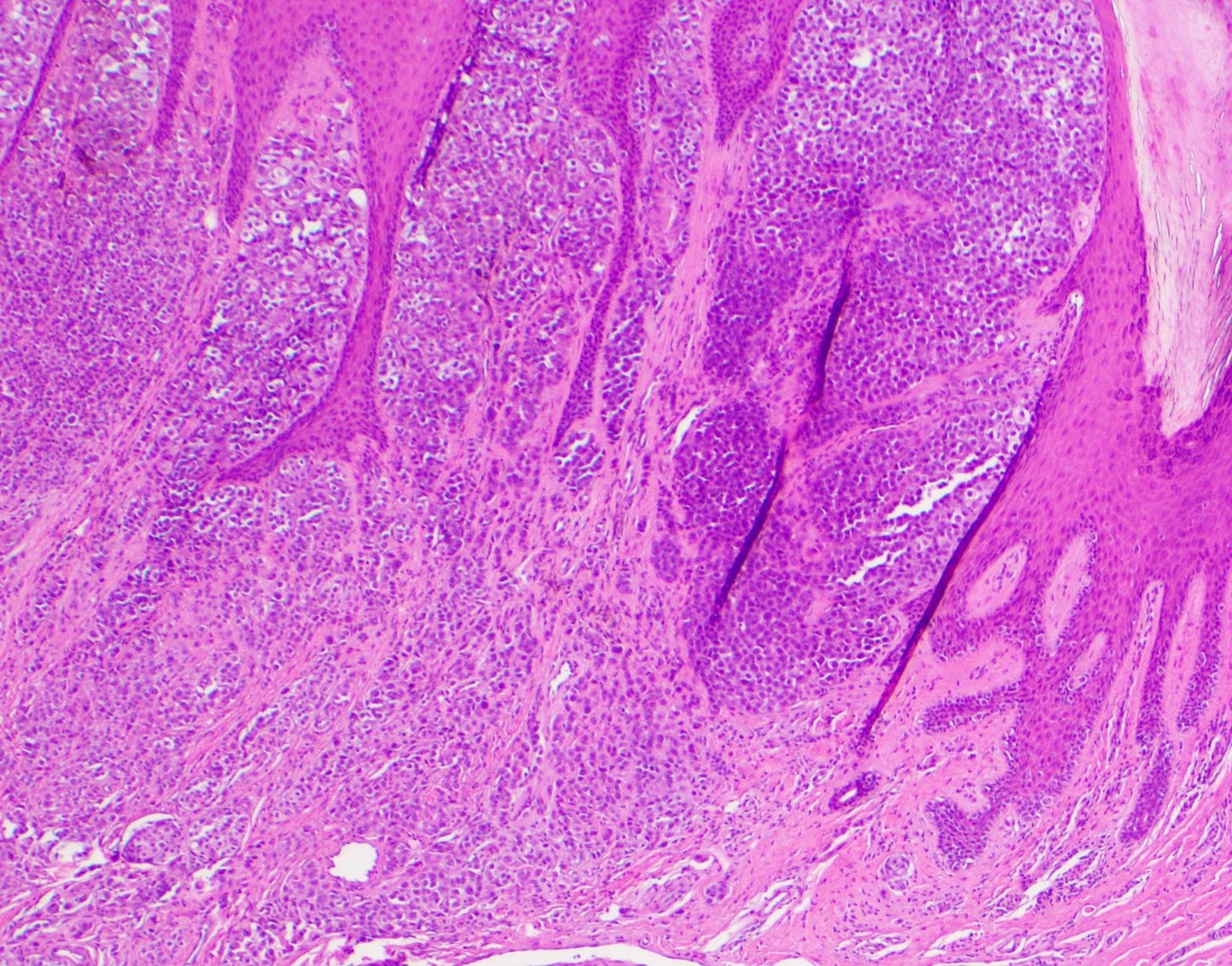
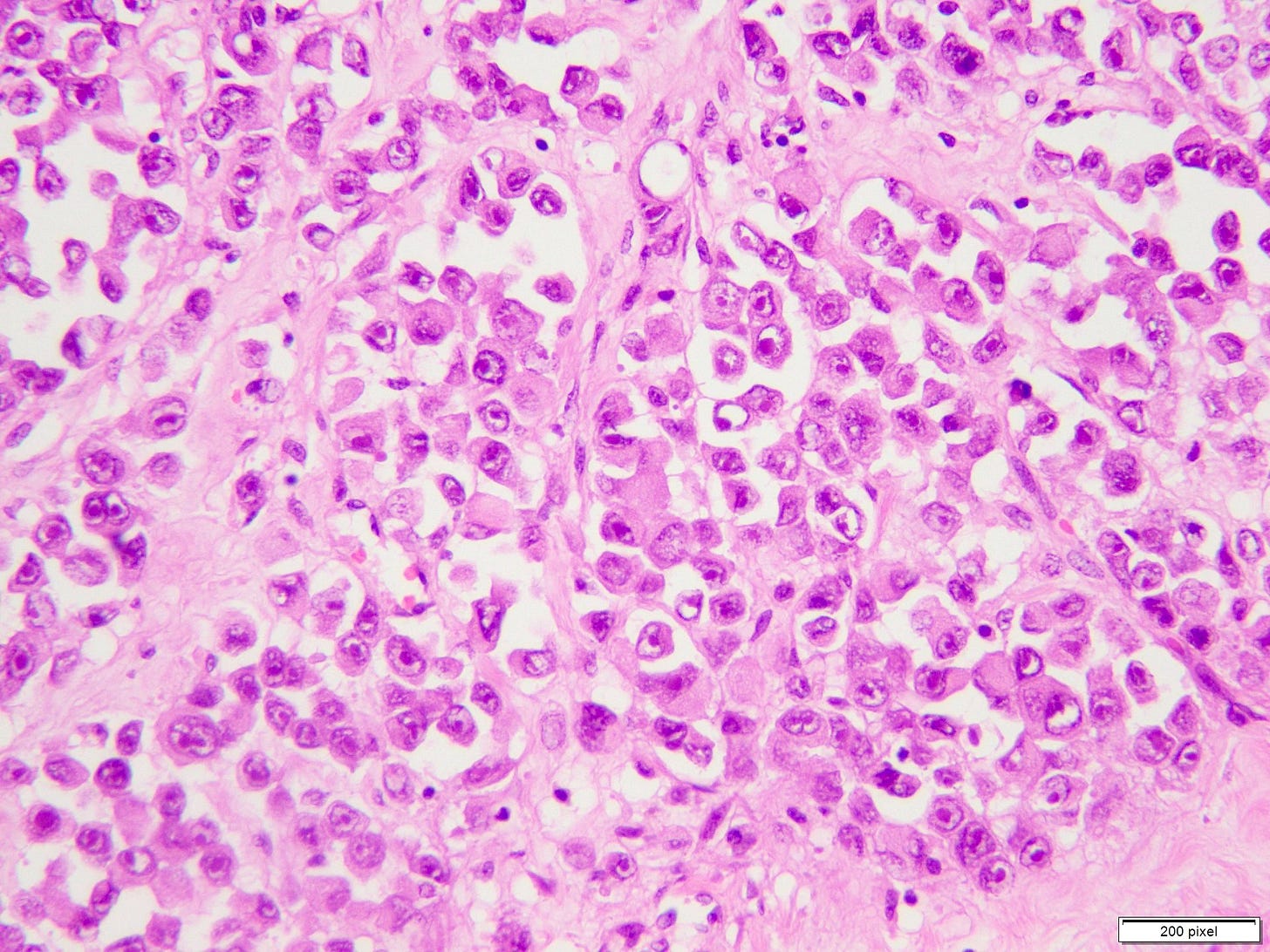
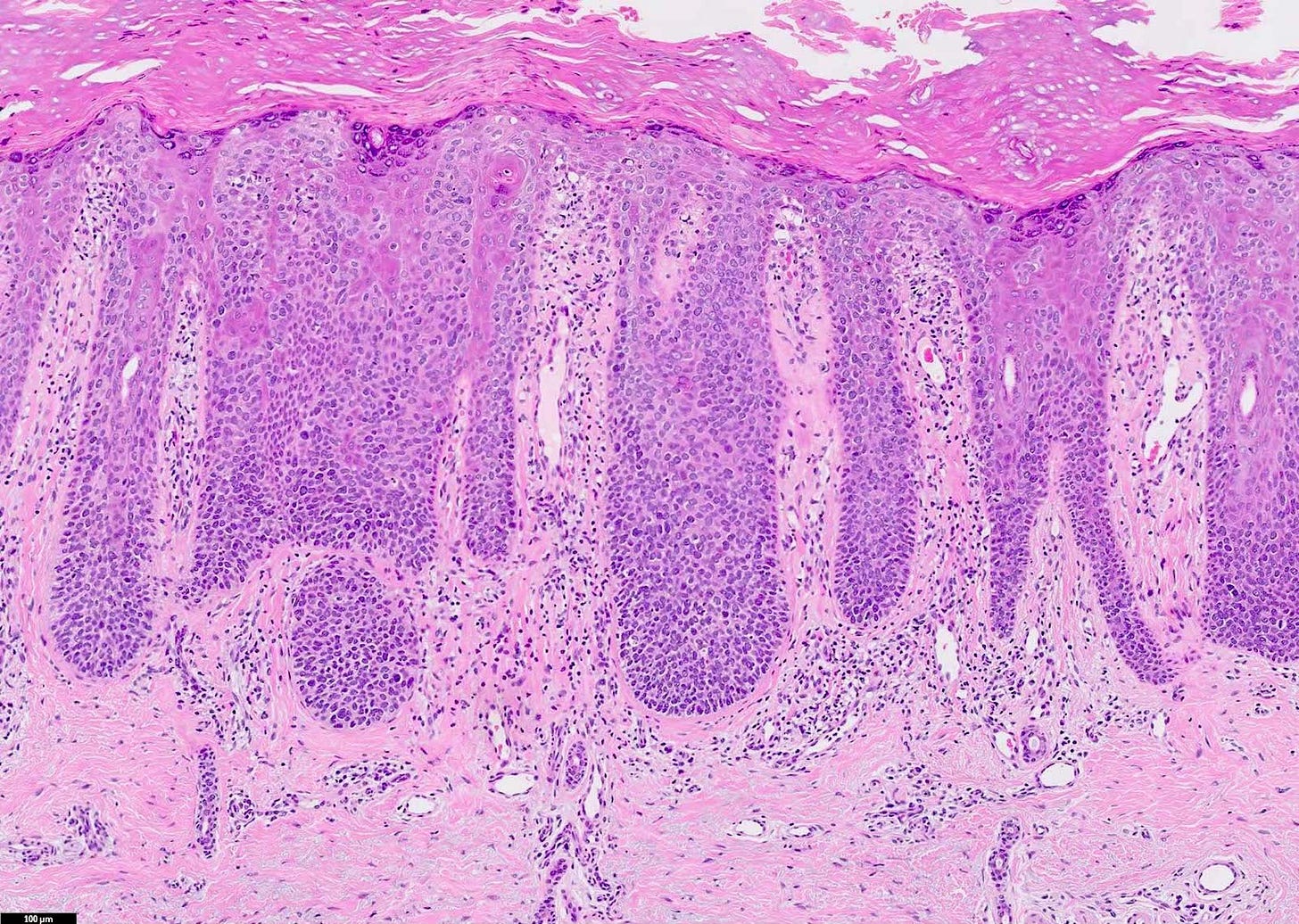
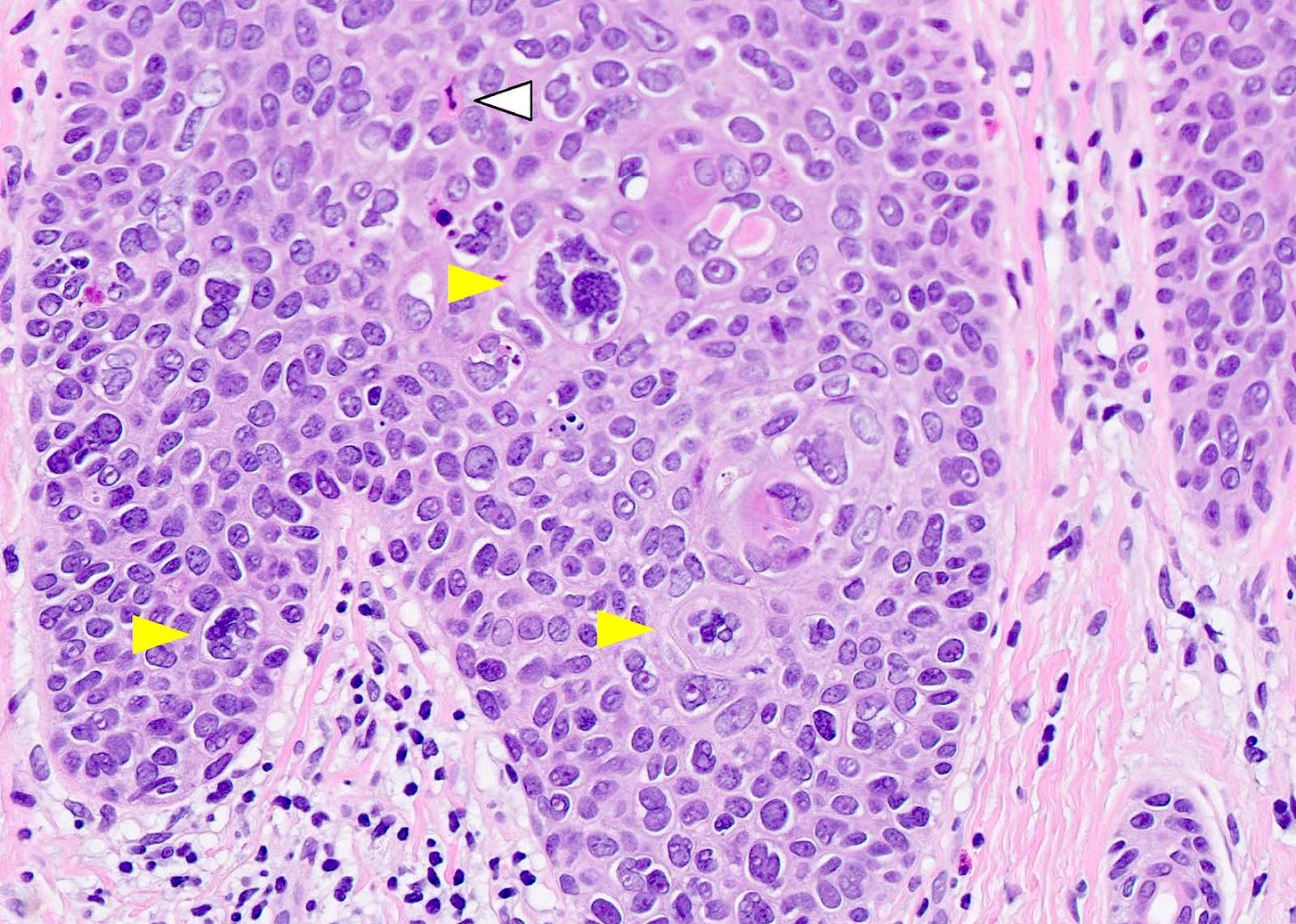
Squamous cell carcinoma in situ is usually found on skin not exposed to sunlight, such as the trunk. It is defined as full thickness keratinocyte atypia with marked nuclear atypia (nuclear hyperchromasia and multinucleation), numerous mitotic figures and atypical mitotic figures.
Squamous cell carcinoma in situ
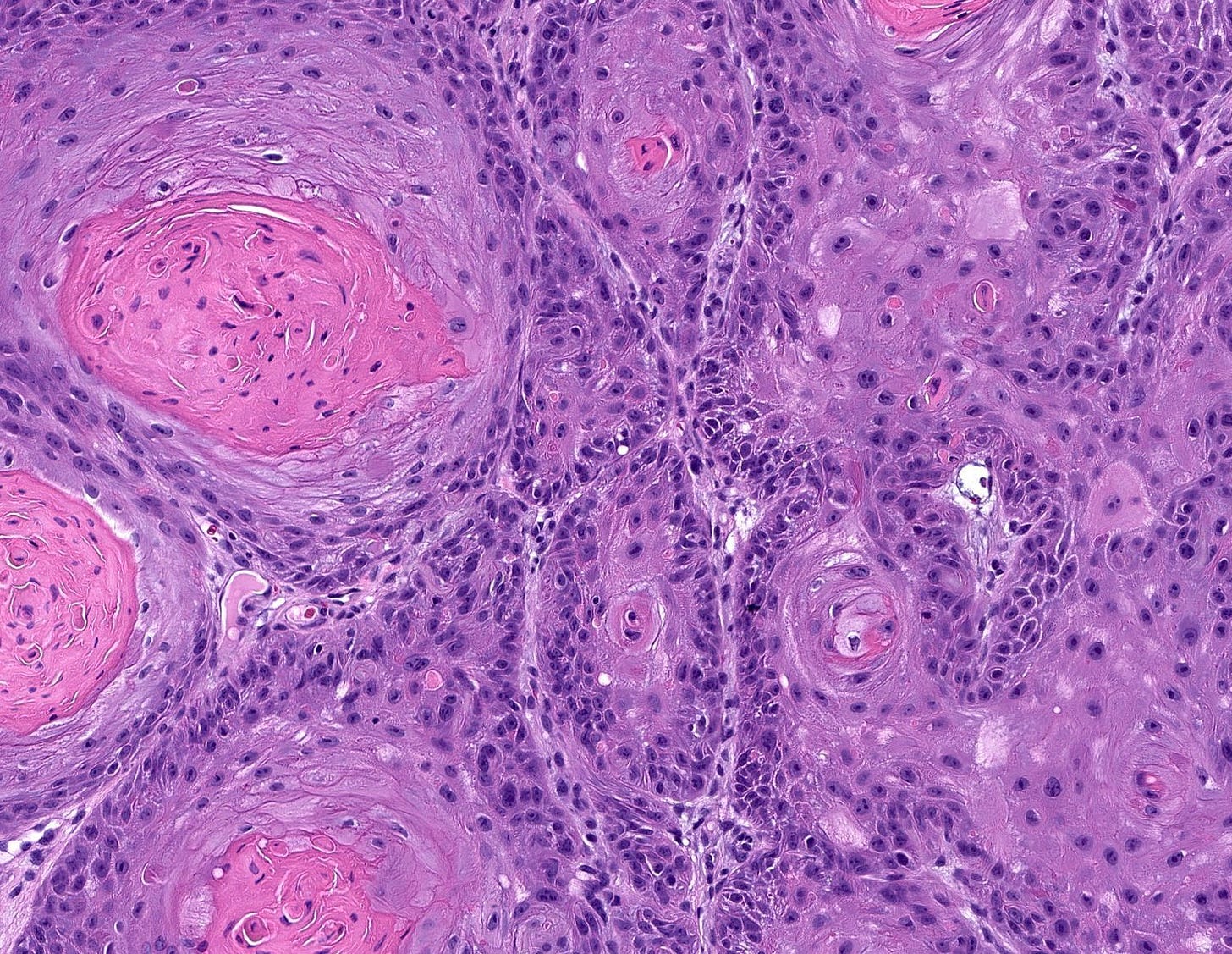
Squamous cell carcinoma is a malignancy of epidermal keratinocytes that displays variable degrees of differentiation and cytological features. It occurs most often in sun exposed areas (scalp, ear, lip, nose, eyelid). It appears to develop through a multistep process, beginning with ultraviolet radiation exposure leading to mutations involving various genes and molecular pathways (Nardo 2020). An associated precursor lesion (actinic keratosis / keratinocytic dysplasia / squamous cell carcinoma in situ) is often present.

Precursors for other skin malignancies
Of the 66 distinct nonmelanotic skin malignancies we have identified in our spreadsheet, only squamous cell carcinoma has a known precursor. What about the other malignancies? We speculate that some may have a molecular precursor with distinct molecular patterns but no morphologic changes. This makes sense considering that some malignancies, such as well differentiated pancreatic adenocarcinoma, appear morphologically similar to normal tissue yet have distinctively different molecular patterns.
The remaining malignancies, as discussed for CNS tumors, may be initiated by a defining mutation in a single stem or progenitor cell that multiplies and acquires additional malignant properties over time. These particular mutations may overcome the limitations on cell division normally imposed by the epithelial structure and progress to malignancy without the need for intraepithelial neoplasia. There is no malignant precursor other than the single cell or a cluster of similar cells at an earlier time in the malignant process, which does not constitute a morphological precursor.
Part 4 will discuss precursors associated with bone, joint & soft tissue malignancies.
If you like these essays, please subscribe or share them with others. These essays will continue to be free. Instead of giving me money, please repost these essays and strive to make our world a better place and to make yourself a better person.
Click here for the Index to Nat’s blog on Cancer and Medicine
Follow us on Substack, LinkedIn, Threads and Instagram (npernickmich) and Tribel (@nat385440b).
Follow our Curing Cancer Network through our Curing Cancer Newsletter, on LinkedIn or Twitter or the CCN section of our PathologyOutlines.com blog. Each week we post interesting cancer related images of malignancies with diagnoses plus articles of interest. Please also read our CCN essays.
Latest versions of our cancer related documents:
American Code Against Cancer (how you can prevent cancer)
Email me at Nat@PathologyOutlines.com - Unfortunately, I cannot provide medical advice.
I also publish Notes at https://substack.com/note. Subscribers will automatically see my Notes.




