In part 1, I shared my journey of discovering my breast cancer and my experiences with the biopsies. In Part 2, I dive into the decision making and steps behind my double mastectomy.
As I mentioned earlier, the biopsy on my right side revealed a grade 3 (high grade) invasive ductal carcinoma that was strongly positive for both estrogen receptor and progesterone receptor. Although the HER2 test came back equivocal (2+), it was ultimately considered negative after a followup FISH molecular test. Given the lack of enough breast tissue for a lumpectomy (common in men) and the fact that the tumor was located near the nipple, the surgeon recommended a right mastectomy to remove all the tissue from that side.
On the left side, the biopsy came back negative, but it was considered "discordant" with the radiology findings. This meant that the biopsy might have missed the area of concern seen on the mammogram. The ultrasound results were also unclear, sometimes showing a mass and at other times not. After discussing the options with my surgeon, we both agreed that a left mastectomy was the best course of action. This would definitively resolve any potential issues on that side as there would be no more breast tissue left to harbor any future problems. Otherwise, I would have to undergo ongoing monitoring for the left side for the rest of my life. Additionally, the procedure for a double mastectomy wasn’t significantly more complex than for a single one, so it seemed like the most straightforward solution.
As part of the surgery, I also had a sentinel lymph node biopsy. The sentinel lymph nodes are the first ones that would drain lymphatic fluid from the tumor and could potentially show signs of metastasis. To locate these nodes, the surgeon injected a radioactive dye into the tumor. This helped pinpoint the sentinel nodes for removal, sparing me from having to undergo the removal of all the lymph nodes on that side. Only one “hot” (radioactive) lymph node was identified and excised.
The initial images below show how my surgeon marked the surgical area on my chest in preparation for the procedure.
The chest was subsequently shaved:
These are the mastectomy specimens that were excised during the surgery, first from the left side, followed by the right. On the right side specimen, you’ll notice a circle drawn around the area where the tumor was located. The sutures, one long and one short, serve to help orient the pathologist when examining the specimen. This is particularly important if the tumor is near one of the margins (edges) of the tissue. In such cases, the surgeon may need to remove additional tissue, but she’ll rely on the marked margins to identify which side of the specimen requires further excision.
This image was taken right after the surgery, showing the mastectomy scars. Below each scar, you can see white circles on both the left and right sides. These mark the spots where drainage tubes were inserted to help remove any fluid that might accumulate during the post-operative period.
The image below was taken a week after the surgery, showing the drainage containers. Each day, I kept track of the amount of fluid in each container. Once the fluid in both containers dropped to 25 cc or less, the drainage tubes were removed.
This was the pathology report for the double mastectomy and sentinel node excision:
PATHOLOGICAL DIAGNOSIS:
A. Left breast, mastectomy, long suture lateral, short suture superior:
- Ductal carcinoma in situ, intermediate nuclear grade, solid and cribriform patterns spanning 8mm.
- Negative resection margins (> 2 mm clearance).
- Gynecomastia, fibrous phase.
- Nipple and skin negative for carcinoma.
B. Right breast, mastectomy, long suture lateral, short suture superior:
- Invasive ductal carcinoma with micropapillary features and foci of necrosis, Nottingham grade 3 (of 3), 20 mm.
- Ductal carcinoma in situ, intermediate nuclear grade, solid and cribriform patterns with focal central necrosis, discontinuously present over a span of 12 mm.
- Negative resection margins.
- Invasive carcinoma is 1.8 mm from deep margin and > 2 mm from other margins.
- Ductal carcinoma in situ is > 2 mm from all margins.
- Nipple and skin negative for carcinoma.
- Biopsy site changes.
C. Right axillary sentinel lymph node/s HOT , biopsy:
- Metastatic mammary carcinoma to one out of one lymph node (1/1).
- Largest metastatic focus measures 10 mm.
- Positive for extranodal extension (< 2 mm).
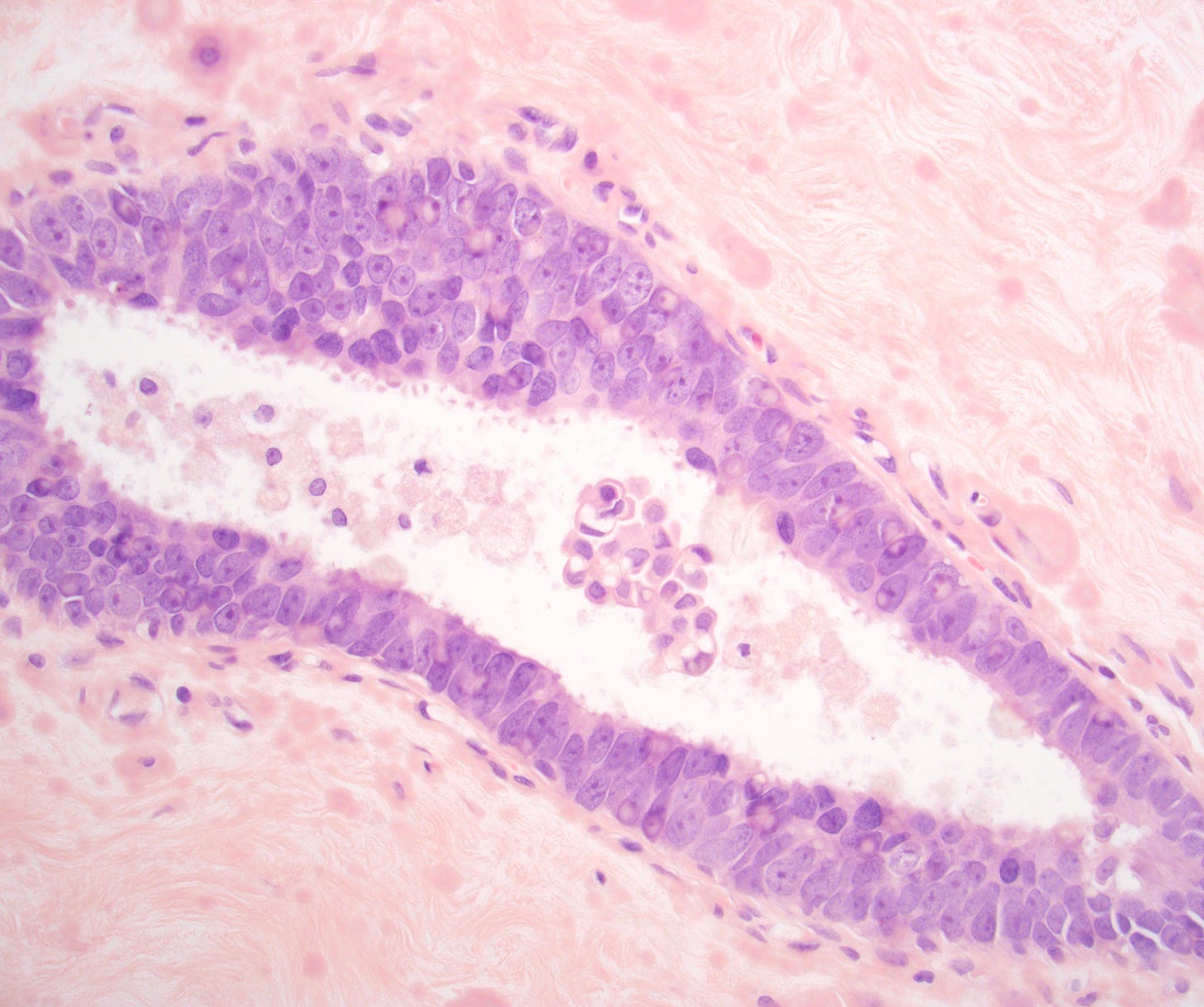
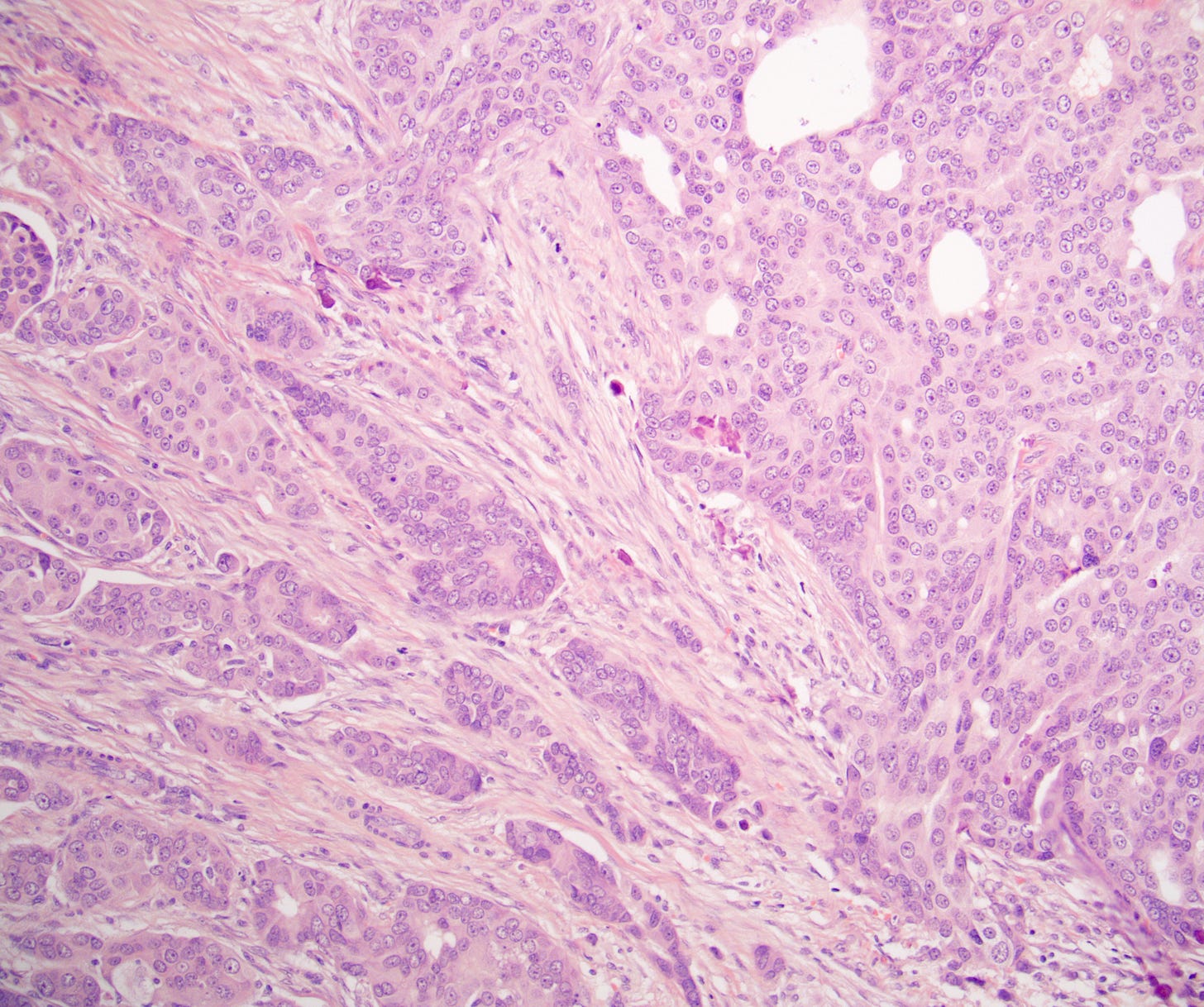
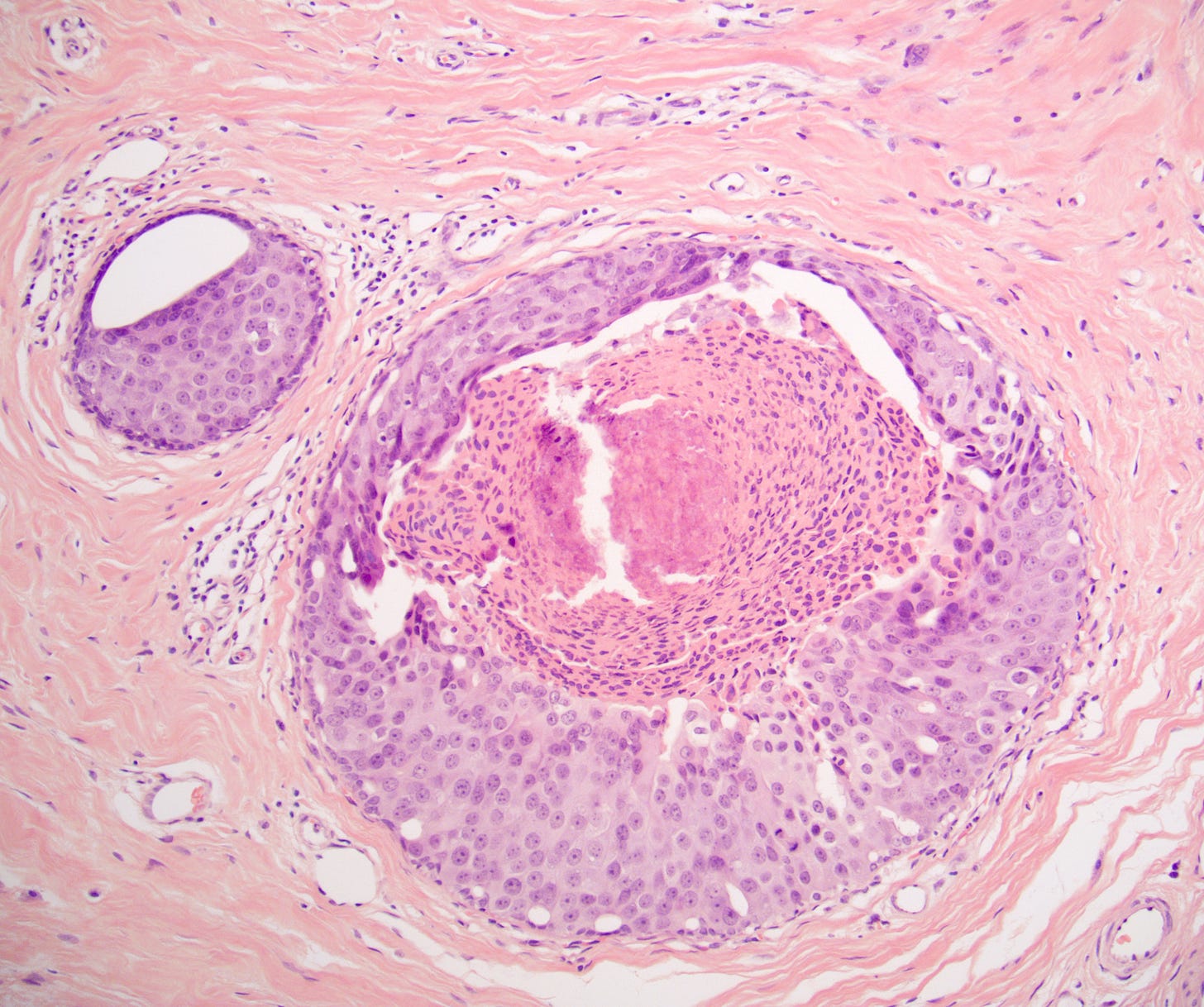
These are the microscopic sections from the mastectomies, first the left side, then the right side, then the sentinel node.
Left breast, mastectomy





Right breast, mastectomy

Right breast, sentinel node excision

The next essay will cover my genetic testing, the molecular testing of my tumor and the radiation therapy that followed.
If you enjoy these essays, please subscribe or share them with others.
Click here for the Index to Nat’s blog on Cancer and Medicine.
Follow me on LinkedIn, Threads and Instagram (@npernickmich) or Bluesky (@natpernick.bsky.social).
Follow our Curing Cancer Network through our Curing Cancer Newsletter, on LinkedIn or in the CCN section of our PathologyOutlines.com blog. Each week we post interesting cancer related images of malignancies with diagnoses plus articles of interest. Please also read our CCN essays.
Latest cancer related documents:
American Code Against Cancer (how you can prevent cancer)
Email: Nat@PathologyOutlines.com (please note I cannot provide medical advice)
Be sure to follow my Substack Notes — subscribers are automatically notified.