Cancer precursor project - breast cancer, part 6g
24 February 2025
This weekly medical blog is scientific, not political. I also publish a daily political blog. Skip any essays or parts of essays of no interest to you - I won’t be offended.
This essay is part of my cancer precursor project that discusses how different types of cancer arise. Part 6 discusses breast cancer:
Part 6a: breast cancer mortality and risk factors and how breast cancer arises.
Part 6b: breast anatomy and histology and invasive breast cancers with known precursors - infiltrating duct carcinoma of no special type, lobular carcinoma and pleomorphic lobular carcinoma.
Part 6c: more invasive breast cancers with known precursors - cribriform carcinoma, secretory carcinoma, neuroendocrine-small cell carcinoma and male invasive breast carcinoma.
Part 6d: more invasive breast cancers with known precursors - tubular carcinoma, triple negative breast cancer, acinic cell carcinoma and metaplastic carcinoma: squamous cell carcinoma.
Part 6d1: more invasive breast cancer with known precursors - encapsulated papillary carcinoma with invasion, solid papillary carcinoma with invasion and intraductal papillary carcinoma with invasion.
Part 6e: invasive breast cancers without known premalignant or preinvasive precursors - BRCA associated carcinoma.
Part 6f: more invasive breast cancers without known premalignant or preinvasive precursors - adenomyoepithelioma with carcinoma, malignant granular cell tumor and malignant phyllodes tumor.
This essay, part 6g, discusses breast cancers without known premalignant or preinvasive precursors and with distinctive, benign appearing cells.
For these four malignancies, risk factors or random events may initially:
Activate networks producing malignant transformation, as well as those that produce glycogen, lipids, oncocytes or sebaceous cells. This activation may occur simultaneously or in response to demands from malignant cells for nutrients or oxygen.
Disturb networks involving glycogen, lipid, mitochondria (oncocytic) or sebaceous cells that, over time, trigger changes to malignant networks. For example, disturbances in the VHL gene, which affects oxygen sensing can cause clear cell renal cell carcinoma.
Disturb both types of networks simultaneously.
Glycogen rich carcinoma
Glycogen rich carcinoma (glycogen rich clear cell carcinoma) is a rare invasive breast carcinoma, first described in 1981, in which at least 90% of the neoplastic cells have abundant clear cytoplasm due to glycogen. It comprises 1 - 3% of breast carcinomas and tends to be high grade with advanced stage and a poor prognosis.
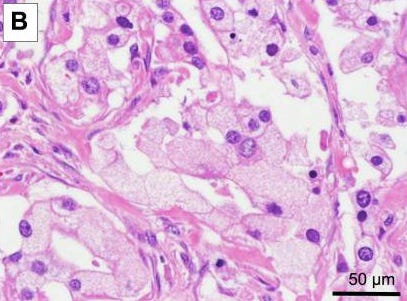
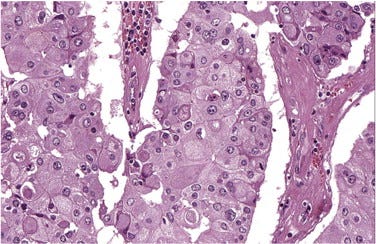
Microscopically, it has solid or papillary patterns of large clear cells with distinct cell borders that may resemble apocrine cells. There are no cytoplasmic vacuoles.
The cytoplasmic glycogen is PAS positive with diastase sensitivity (i.e., PAS stains the cells but the stain is removed after applying diastase, suggesting the presence of glycogen). These tumors are negative for lipids and are often triple negative (i.e., negative for ER, PR and HER2, although there are exceptions).
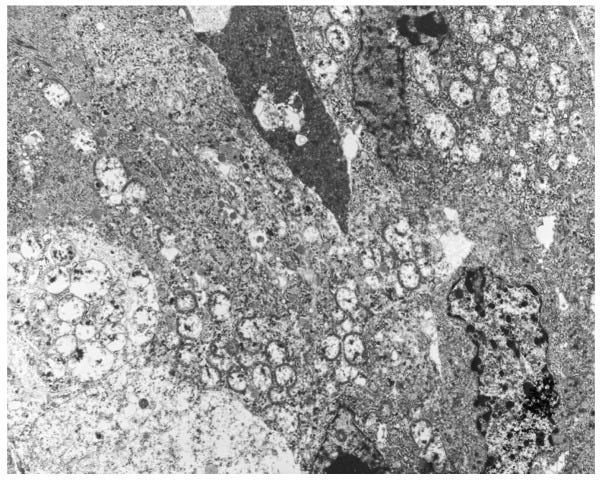
Electron microscopy confirms the presence of non membrane bound glycogen and empty glycogen lakes.
Recommended treatment is mastectomy with sentinel lymph node biopsy or axillary dissection, regardless of the tumor size. Radiation therapy appears to improve prognosis.
Glycogen rich breast carcinoma arises without an apparent precursor, based on mechanisms that may be similar to glycogen rich or clear cell carcinomas of the bladder, cervix, kidney, liver and ovary.
Glycogen is a highly branched polymer of glucose used to store and release energy in the brain, liver, heart and muscle.
However, glycogen metabolism may be hijacked during malignant transformation, as demonstrated by higher levels in malignant cells than in surrounding tissues. What initiates this is unknown.
Glycogen dysregulation affects cancer cell proliferation, migration and invasion.
Molecular alterations in the chromatin remodeling machinery and other pathways are common to these tumors.
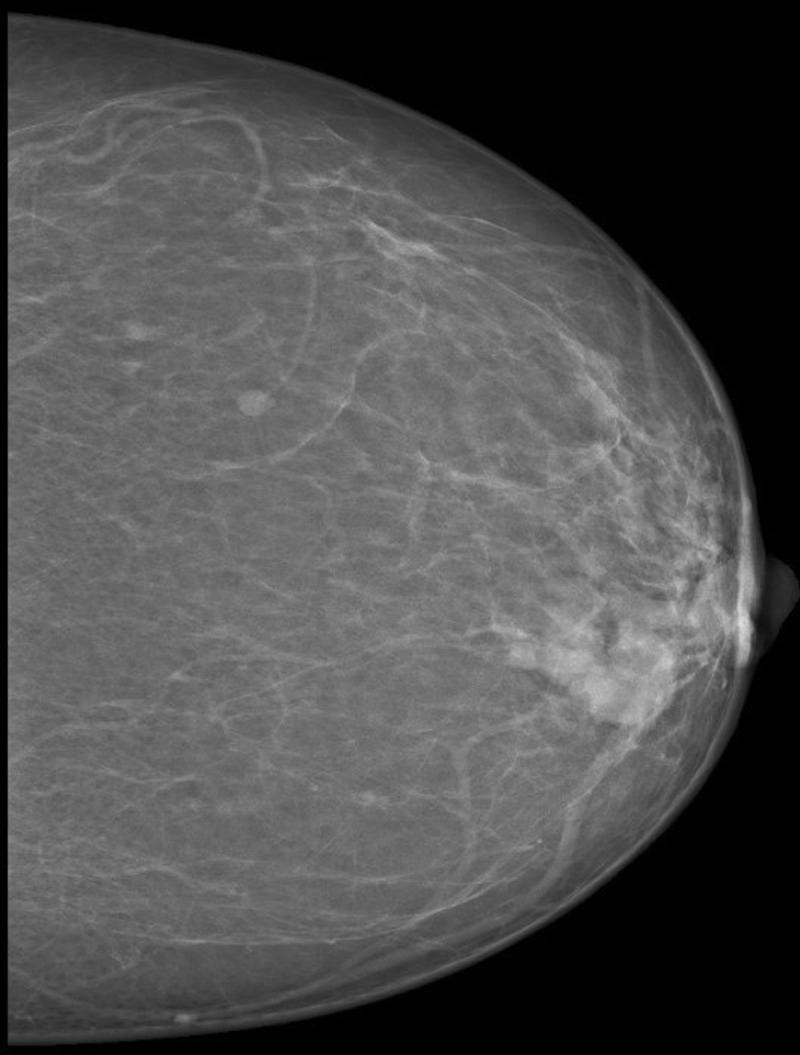
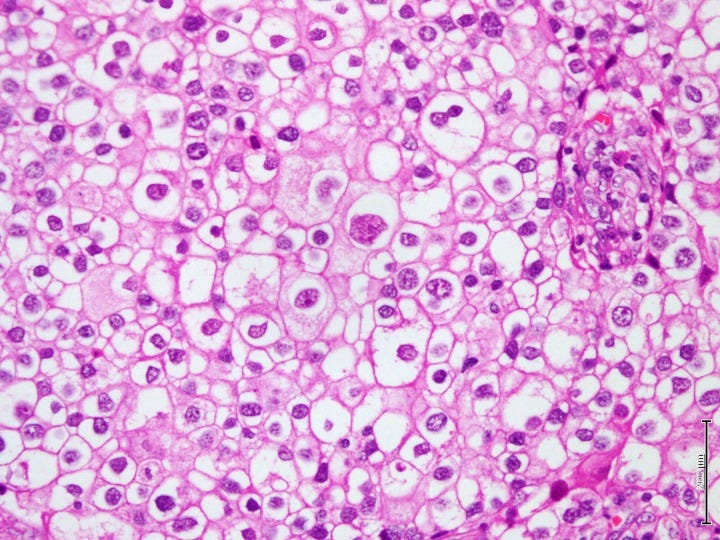
Glycogen rich carcinoma - radiologic and microscopic images
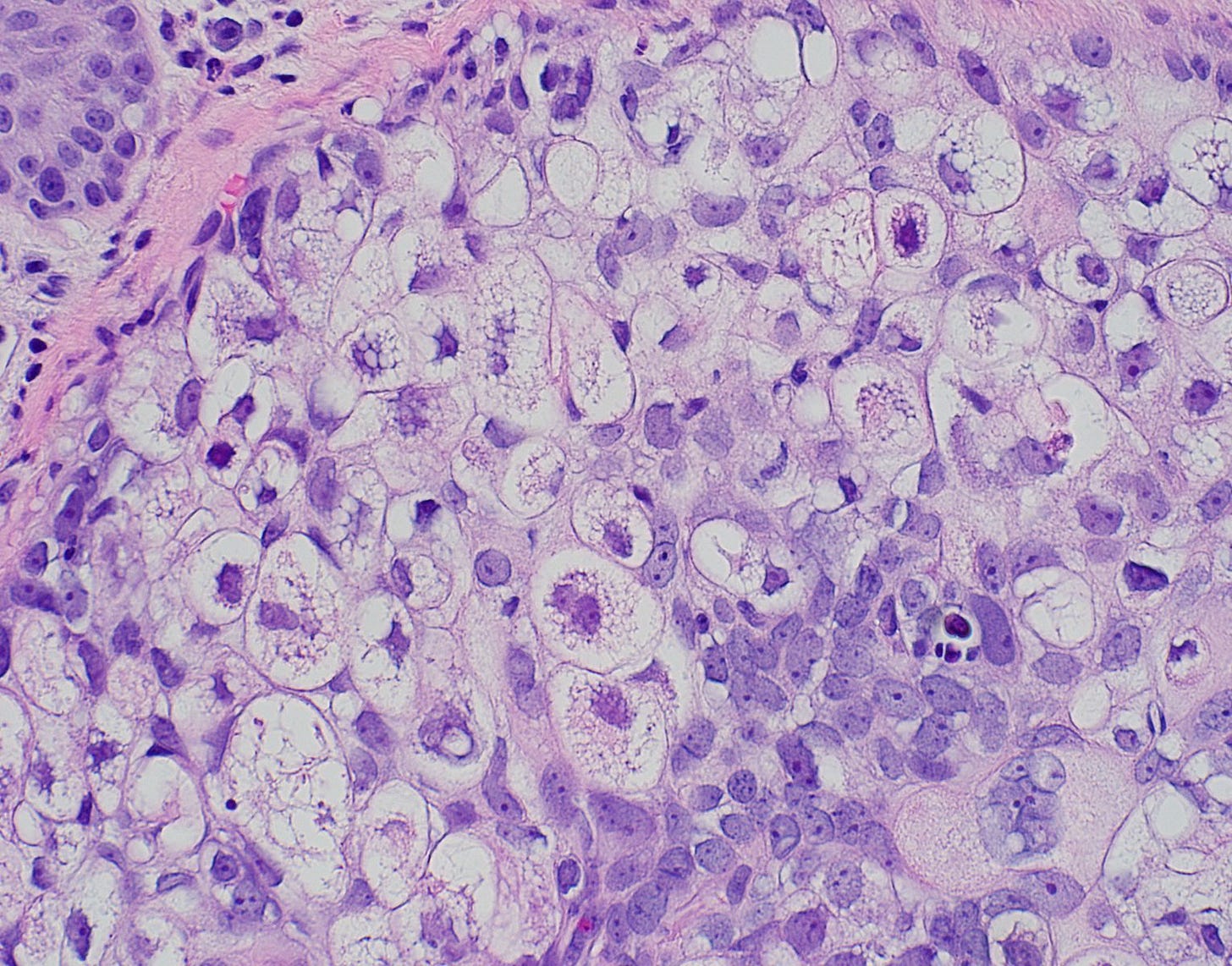
Lipid rich carcinoma
Lipid rich carcinoma is a rare invasive breast carcinoma in which at least 90% of the neoplastic cells have prominent intracytoplasmic neutral lipids. It comprises 1 - 2% of breast carcinomas and tends to have a poor prognosis due to frequent (70%) nodal metastases at presentation.
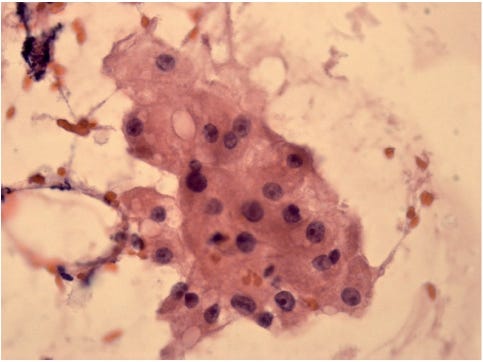
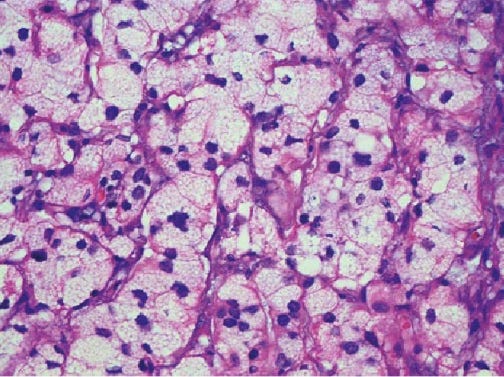
Microscopically, it has nests, cords and sheets of large polygonal cells with foamy or vacuolated cytoplasm containing lipid. These cells may resemble the clear cells of glycogen rich carcinoma or lipoblasts. The nuclei are irregular with coarse chromatin, moderate atypia and prominent nucleoli.
The tumor cells stain with lipid stains (Sudan black and Oil red O) on fresh tissue. They usually are HER2+ (71%+) but negative for ER, PR, glycogen (PAS) and mucin.
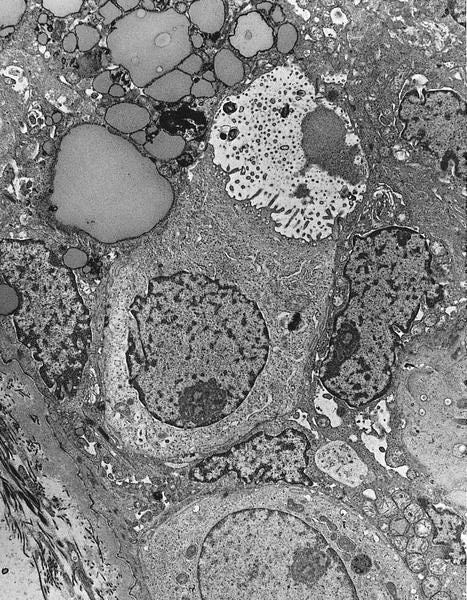
Electron microscopy shows numerous intracytoplasmic non membrane bound lipid droplets, often within autophagocytic vacuoles.
Lipid rich carcinoma does not appear to have any premalignant precursors and its pathogenesis is unknown. However, lipid mediators, including lipid droplets, may be biomarkers for cancer onset, progression or resistance. Breast cancer may exhibit metabolic plasticity that allows cancer cells to choose the best metabolic program to sustain tumor progression, choosing between lipid metabolism, glycolysis (the Warburg effect) and oxidative phosphorylation with mitochondria.
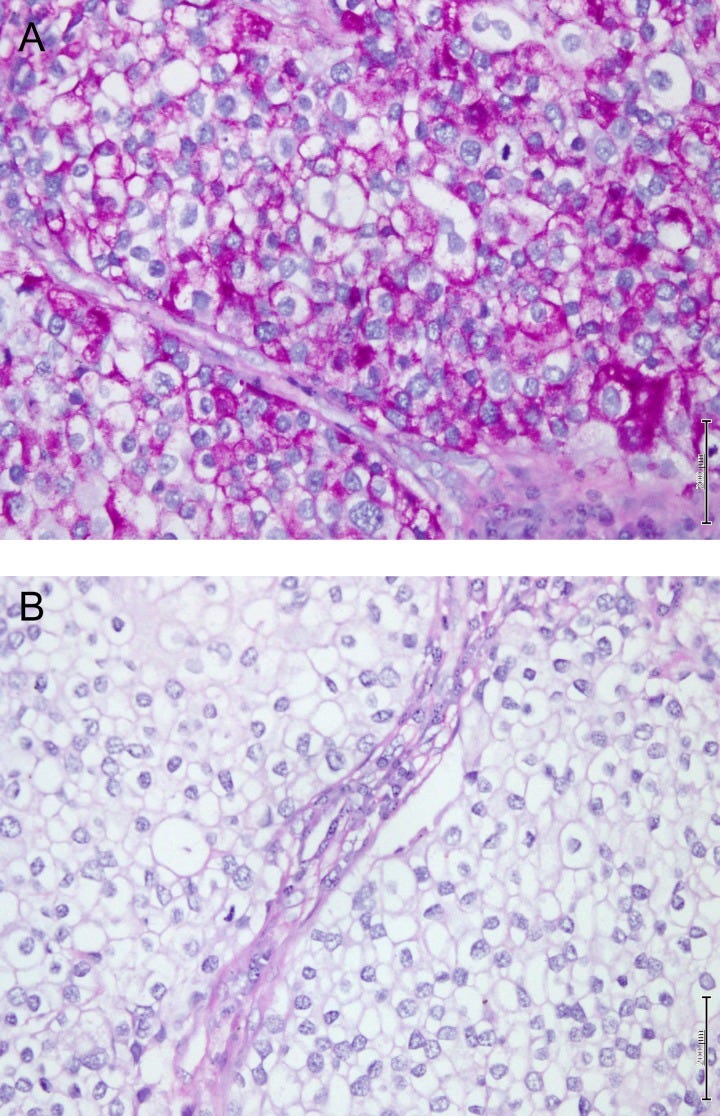
Lipid rich carcinoma - microscopic, cytologic and electron microscopy images

Oncocytic carcinoma
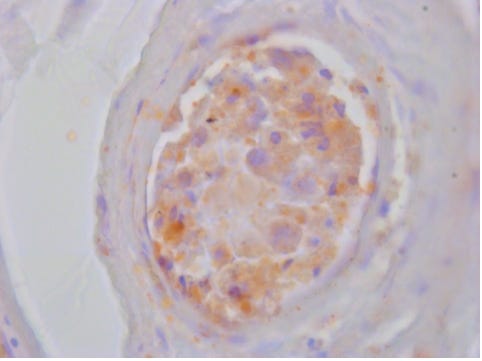
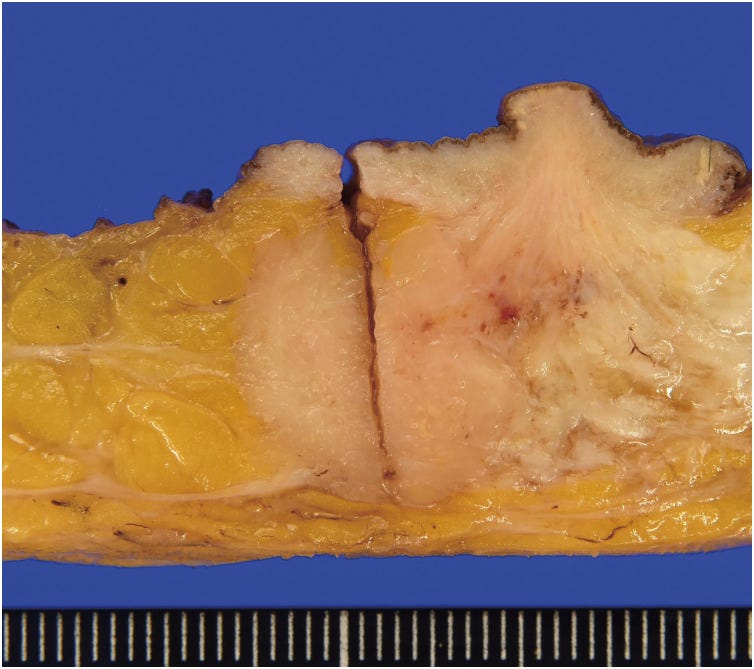
Oncocytic carcinoma is an invasive breast carcinoma in which at least 70% of the neoplastic cells are oncocytic; i.e. large with deeply acidophilic (eosinophilic) granular cytoplasm, often due to the accumulation of mitochondria. It is very rare and comprises < 1% of breast carcinomas. It may resemble apocrine carcinoma, but oncocytic carcinoma cells stain with antimitochondrial antibodies and are negative for GCDFP-15 and androgen receptor (apocrine carcinoma cells stain opposite). Oncocytic carcinoma is often high grade (grade 3) at presentation and HER2+. It tends to have a poor prognosis but its overall survival is similar to infiltrating ductal carcinoma when matched for grade and stage.
Electron microscopy shows that oncocytic cells are enlarged and granular due to an increase in the number and size of mitochondria.
Oncocytic carcinoma does not appear to have any premalignant precursors. It may be associated with oncocytic changes in nonneoplastic epithelium and oncocytic changes may be due to senescence. It frequently exhibits gains of 11q13.1–13.2 and 19p13, similar to oncocytic tumors of the kidney and thyroid.
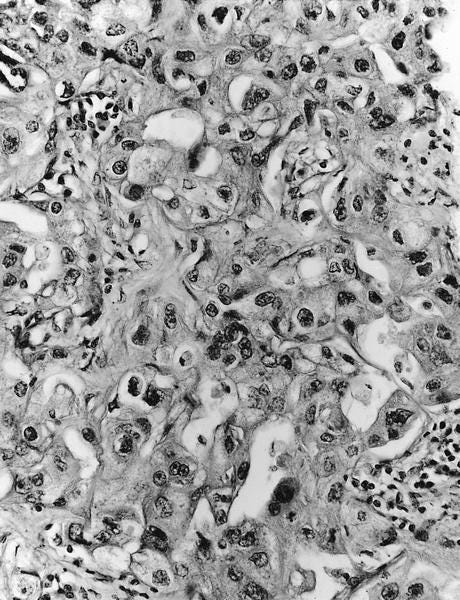
Oncocytic carcinoma - clinical, gross, microscopic and electron microscopy images





Sebaceous carcinoma
Sebaceous carcinoma of the breast is a malignant neoplasm with sebaceous differentiation. It is more commonly described in the skin and eye and is extremely rare in the breast.
There is no association with microsatellite instability or Muir-Torre syndrome as with sebaceous neoplasms in other organs.
Its clinical features are very similar to those of breast fibroadenoma and it may be removed as a benign lesion. However, it has lymph node metastasis in 50% of cases. A recent study suggested that it has a high potential for recurrence and recommended that patients with hormone receptor positive disease receive endocrine therapy.
Diagnosis requires that 50% or more of the tumor has sebaceous differentiation with no evidence of cutaneous derivation. The tumors are composed of cords, lobules and solid sheets of cells with abundant vacuolated cytoplasm, reminiscent of mature sebocytes. Nuclei vary from relatively small monomorphic and darkly stained to large and pleomorphic with a more vesicular appearance and prominent basophilic or slightly eosinophilic nucleoli. The nuclei are mostly eccentrically located and scalloped by the intracytoplasmic vacuoles.
Cytological examination reveals atypical cells presenting predominantly as loose clusters, but with no tubular or papillary structures or mucin production. Papanicolaou-stained smears show differentiated tumor cells within yellowish clusters.
Positivity for ER is 64.7%, PR 58.8%, HER2 13.3%, p53 66.7%, EMA 88.9% and GCDFP-15 0%.
Sebaceous carcinoma does not appear to have any premalignant precursors. Its origin is unknown but may be due to a ductal reserve cell capable of sebaceous differentiation or the displacement of an embryonic group of epidermal cells in the breast parenchyma.
Sebaceous carcinoma - gross, microscopic and electron microscopy images
The next essay, part 6h, will discuss other breast cancers without known precursors.
If you like these essays, please subscribe or share them with others.
Click here for the Index to Nat’s blog on Cancer and Medicine.
Follow me at https://www.linkedin.com/in/nat-pernick-8967765/ (LinkedIn), npernickmich (Threads and Instagram), natpernick.bsky.social (Bluesky) or @nat385440b (Tribel).
Follow our Curing Cancer Network through our Curing Cancer Newsletter, on LinkedIn or the CCN section of our PathologyOutlines.com blog. Each week we post interesting cancer related images of malignancies with diagnoses plus articles of interest. Please also read our CCN essays.
Latest versions of our cancer related documents:
American Code Against Cancer (how you can prevent cancer)
Email me at Nat@PathologyOutlines.com - Unfortunately, I cannot provide medical advice.
I also publish Notes at https://substack.com/note. Subscribers will automatically see my Notes.




