Cancer precursor project - breast cancer, part 6h
5 March 2025
This weekly medical blog is scientific, not political. I also publish a daily political blog. Skip any essays or parts of essays that you find too technical or are not interested in - I won’t be offended.
This essay is part of my cancer precursor project that discusses how different types of cancer arise. Part 6 discusses breast cancer and its 45 separate types:
Part 6a: breast cancer mortality and risk factors and how breast cancer arises.
Invasive breast cancers with known precursors:
Part 6b: breast anatomy and histology, infiltrating duct carcinoma of no special type, lobular carcinoma and pleomorphic lobular carcinoma.
Part 6c: cribriform carcinoma, secretory carcinoma, neuroendocrine-small cell carcinoma and male invasive breast carcinoma.
Part 6d: tubular carcinoma, triple negative breast cancer, acinic cell carcinoma and metaplastic carcinoma: squamous cell carcinoma.
Part 6d1: encapsulated papillary carcinoma with invasion, solid papillary carcinoma with invasion and intraductal papillary carcinoma with invasion.
Invasive breast cancers without premalignant or preinvasive precursors:
Part 6e: BRCA associated carcinoma.
Part 6f: adenomyoepithelioma with carcinoma, malignant granular cell tumor and malignant phyllodes tumor.
Part 6g: glycogen rich carcinoma, lipid rich carcinoma, oncocytic carcinoma and sebaceous carcinoma.
Part 6h discusses two invasive breast carcinomas without premalignant or preinvasive precursors although there are DCIS subtypes with similar patterns:
For completeness, these are the other major DCIS subtypes and their relationship to invasive breast carcinoma:
DCIS subtypes that are precursors for specific invasive carcinomas:
Cribriform DCIS is a precursor of cribriform carcinoma, see part 6c.
Papillary DCIS is a precursor of encapsulated papillary carcinoma, see part 6d1.
Solid DCIS is a precursor of solid papillary carcinoma with invasion, see part 6d1.
DCIS subtypes that are not associated with specific invasive carcinomas:
Comedo DCIS
Cystic hypersecretory DCIS - this rare form of DCIS is rarely associated with microinvasive cystic hypersecretory carcinoma (this invasive disease is not part of the WHO classification of breast cancer).
Flat or clinging DCIS
Squamous DCIS - of note, although squamous DCIS is not associated with a specific invasive carcinoma, squamous dysplasia IS associated with metaplastic carcinoma, see part 6d.
Apocrine carcinoma
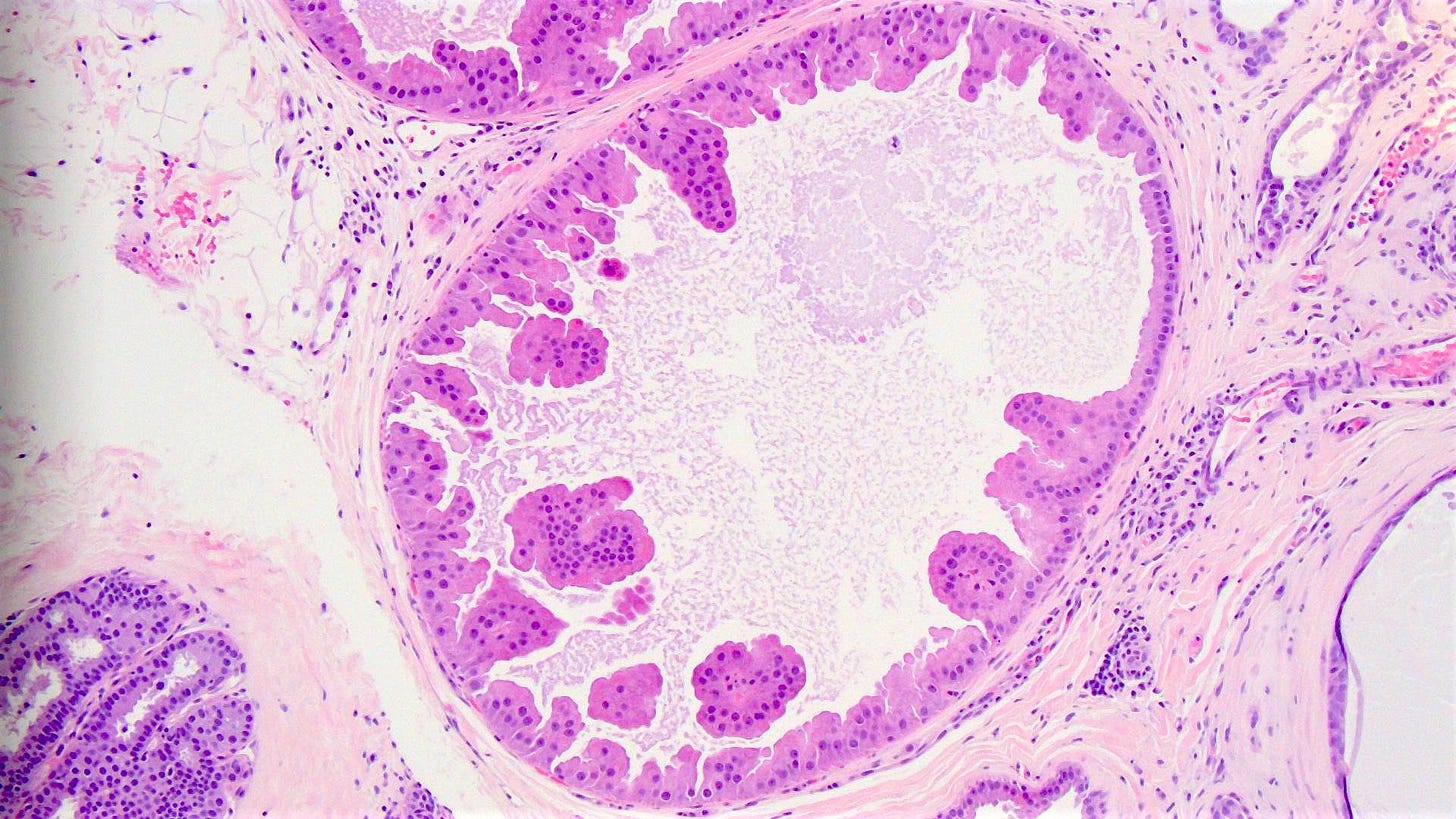
Apocrine carcinoma is a rare invasive breast carcinoma in which at least 90% of tumor cells have apocrine morphology. The malignant cells are large with abundant eosinophilic and granular cytoplasm, enlarged nuclei and prominent nucleoli. Tumor cells are typically high grade and poorly differentiated. Apocrine carcinoma may be associated with ductal carcinoma in situ (DCIS) with apocrine features but this is not considered to be a precursor.
Apocrine carcinoma represents 1% of invasive breast cancers. Although most of these tumors are sporadic, some occur in patients with germline PTEN mutations (Cowden syndrome). Clinically and radiologically, they are similar to invasive breast cancer of no special type (NST) and present with a firm, poorly circumscribed mass.
These tumors are typically triple negative (estrogen receptor (ER) negative, progesterone receptor (PR) negative, HER2 negative) and are androgen receptor (AR) positive.
Triple negative cases of apocrine carcinoma may be a special subtype of triple negative breast cancer but with a better short term prognosis.
Treatment includes surgical excision and possibly radiation therapy, dependent on stage. Patients may have a poor response to neoadjuvant chemotherapy. Anti-HER2 therapy is given for HER2+ tumors.
Apocrine carcinoma may arise from the malignant transformation of apocrine metaplasia, seen commonly in fibrocystic changes of the breast. However, apocrine metaplasia is NOT considered a risk factor for invasive apocrine carcinoma. Apocrine carcinoma is most commonly associated with mutations to the PIK3CA / PTEN / AKT pathway and TP53.
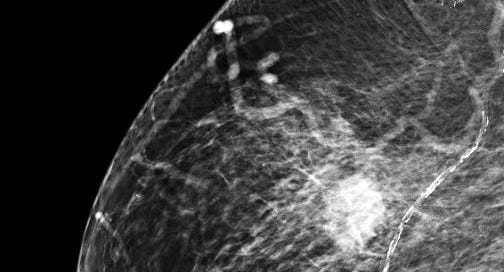
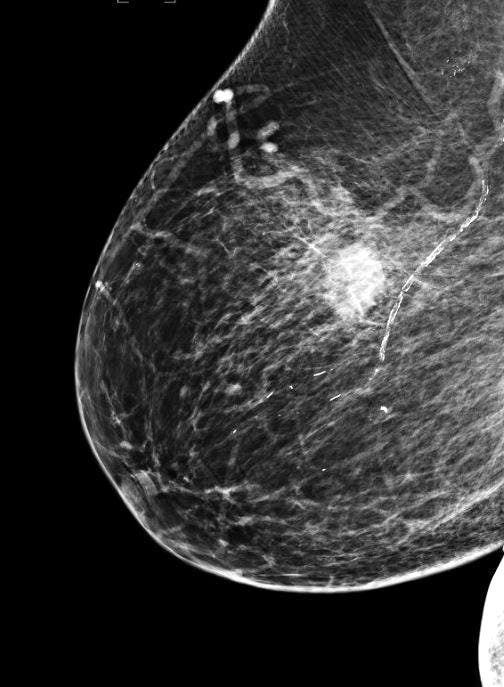
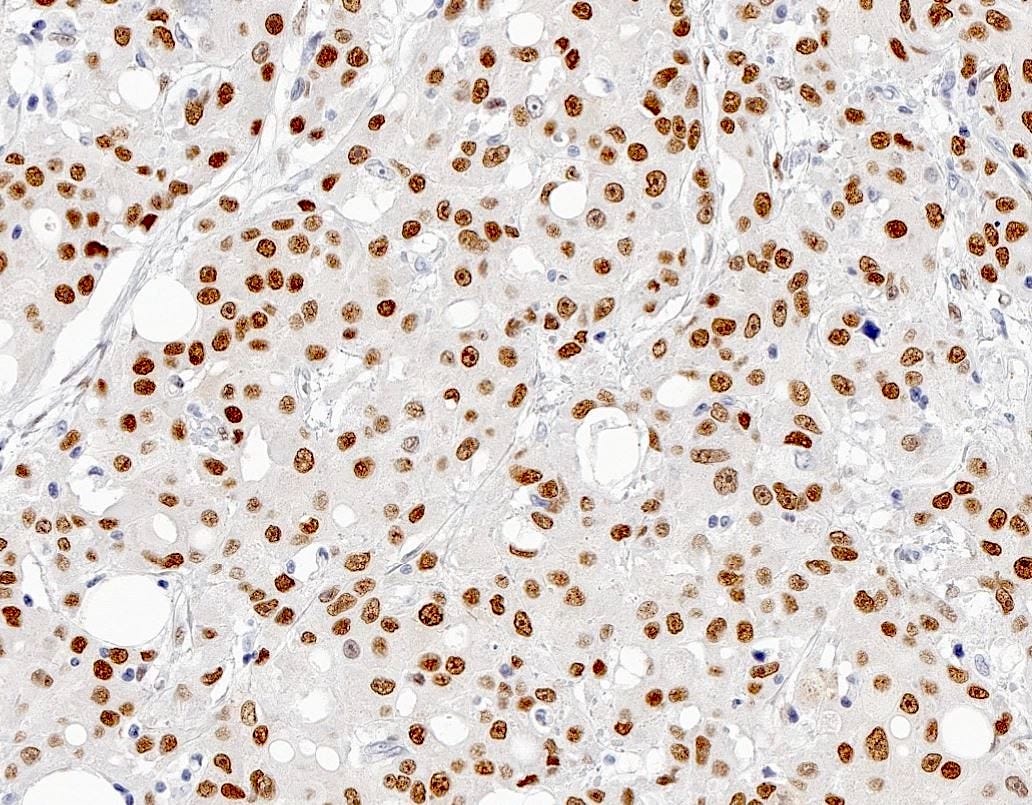
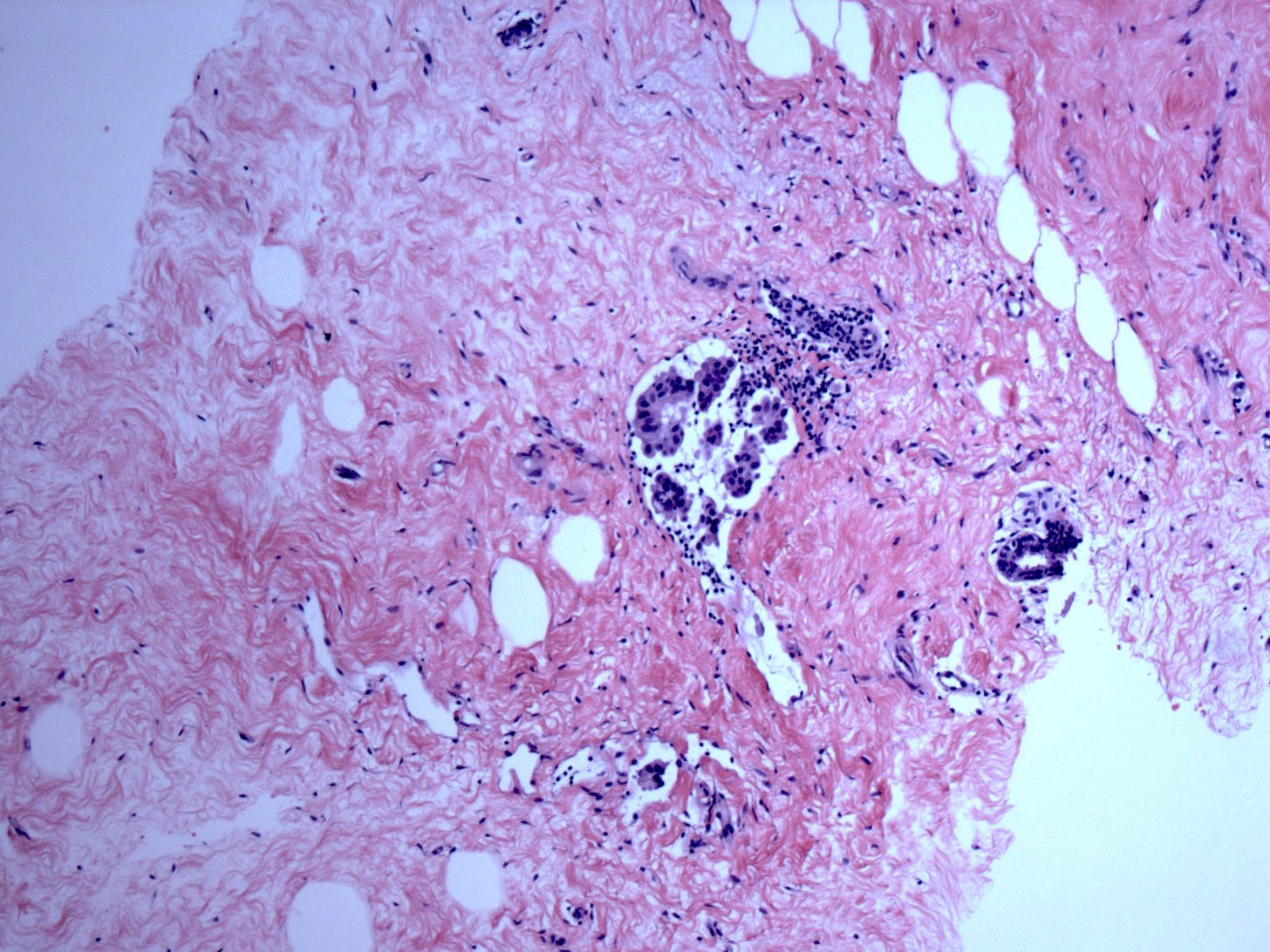
Apocrine carcinoma - radiologic and microscopic images
Invasive micropapillary carcinoma
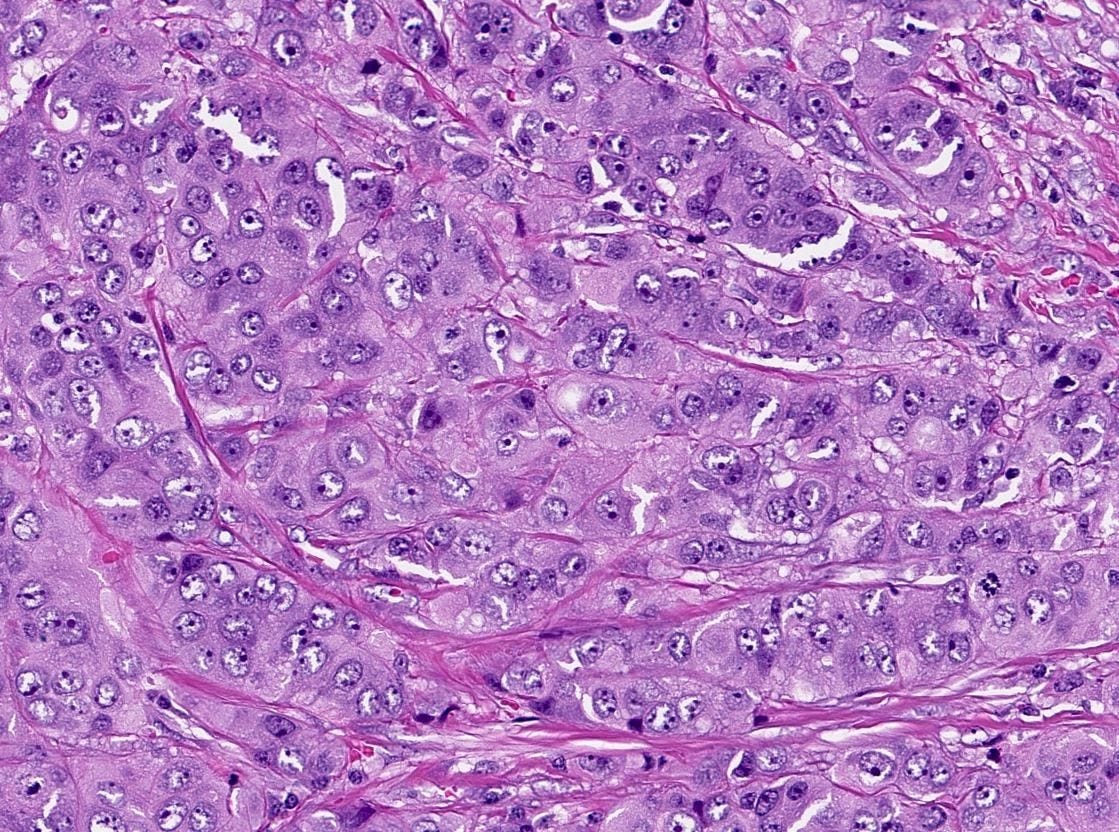
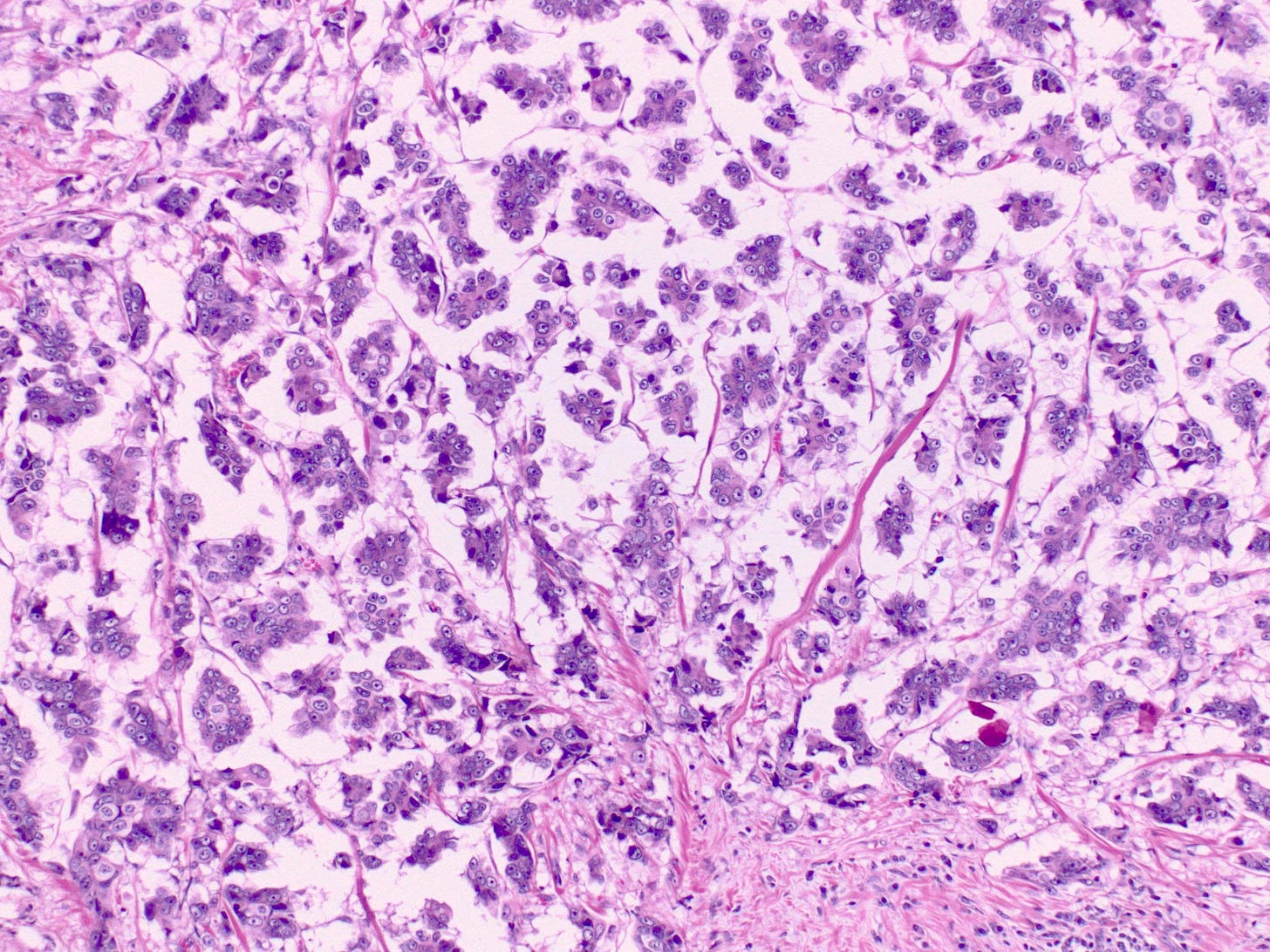
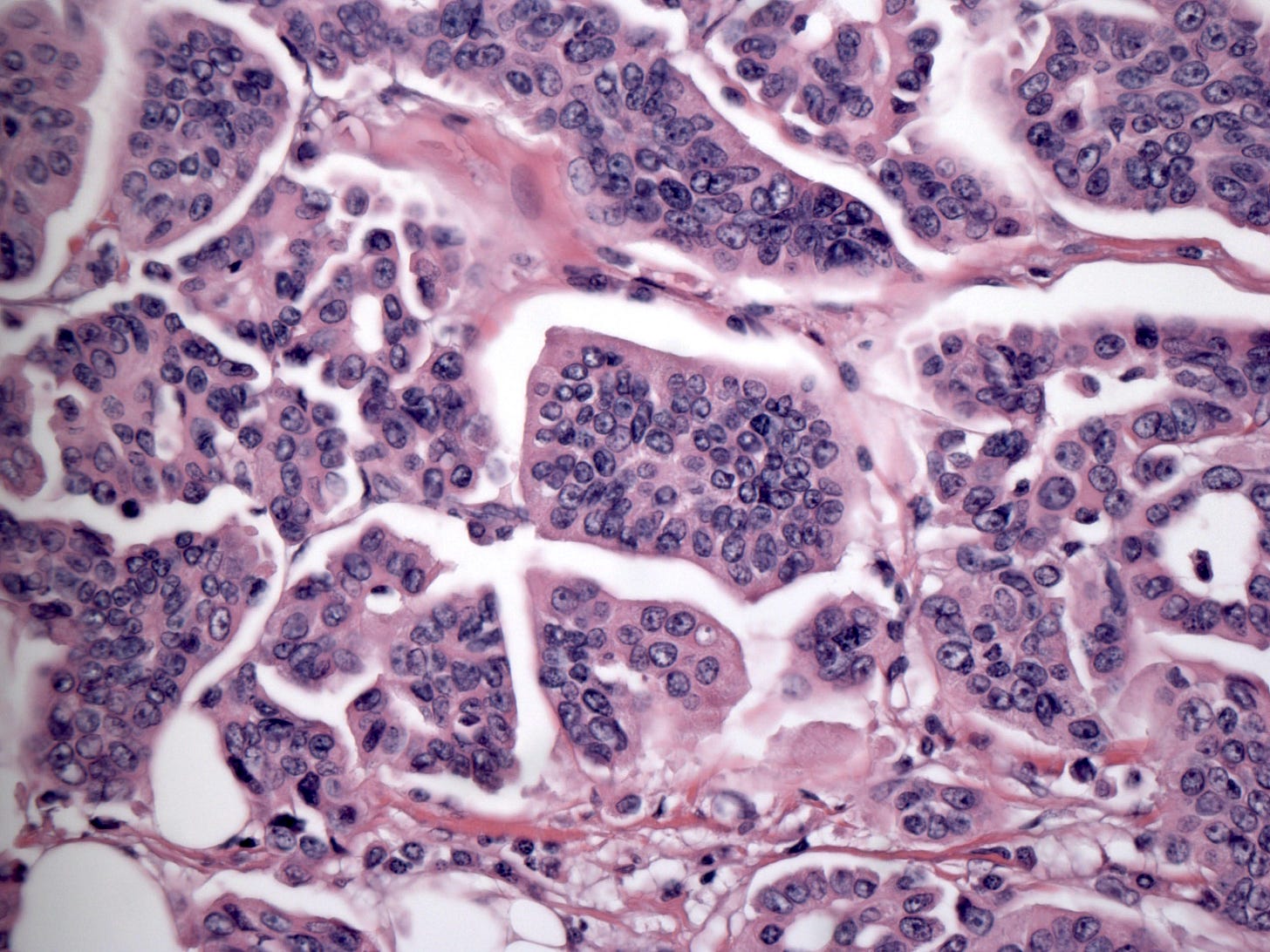
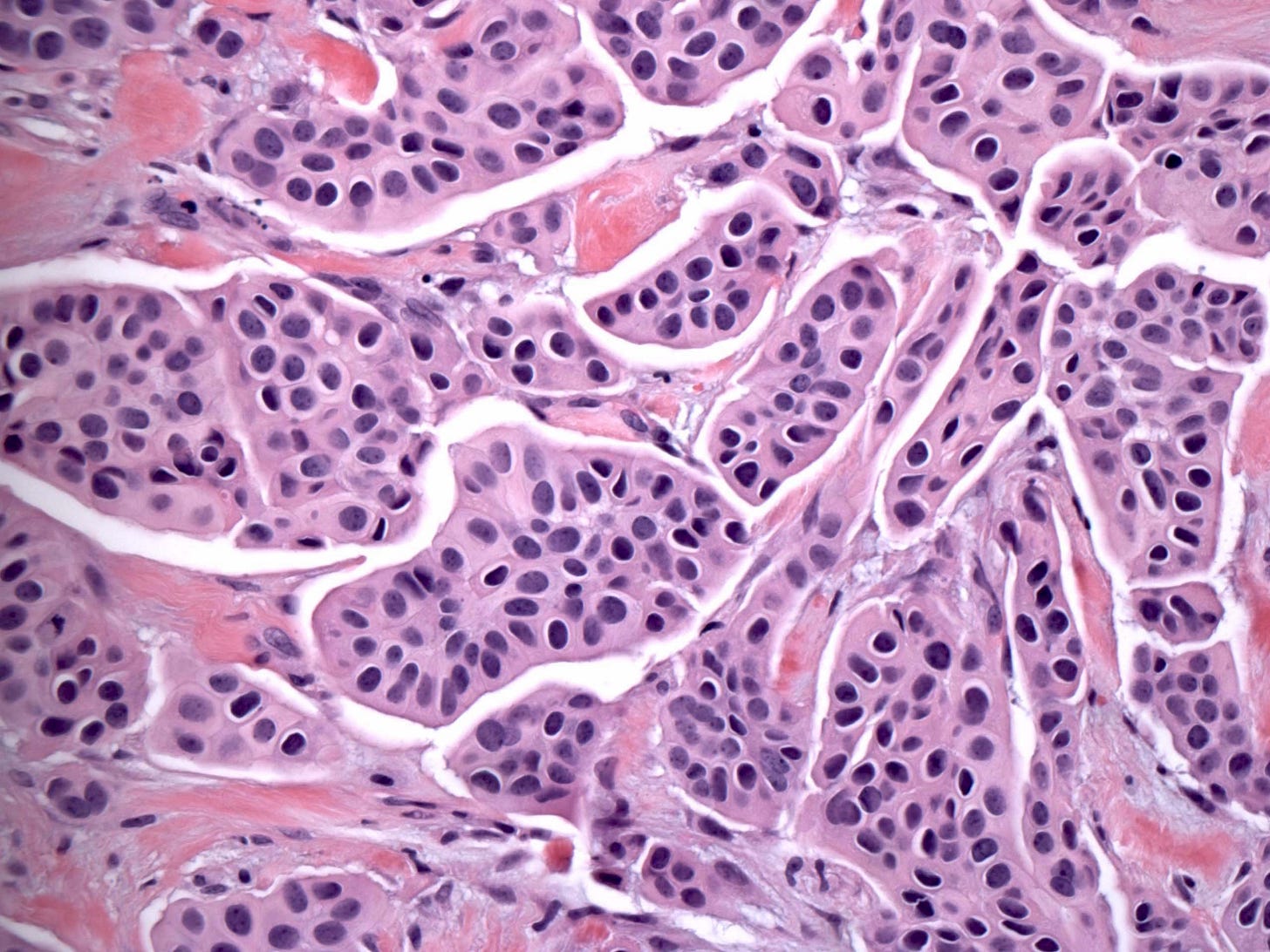
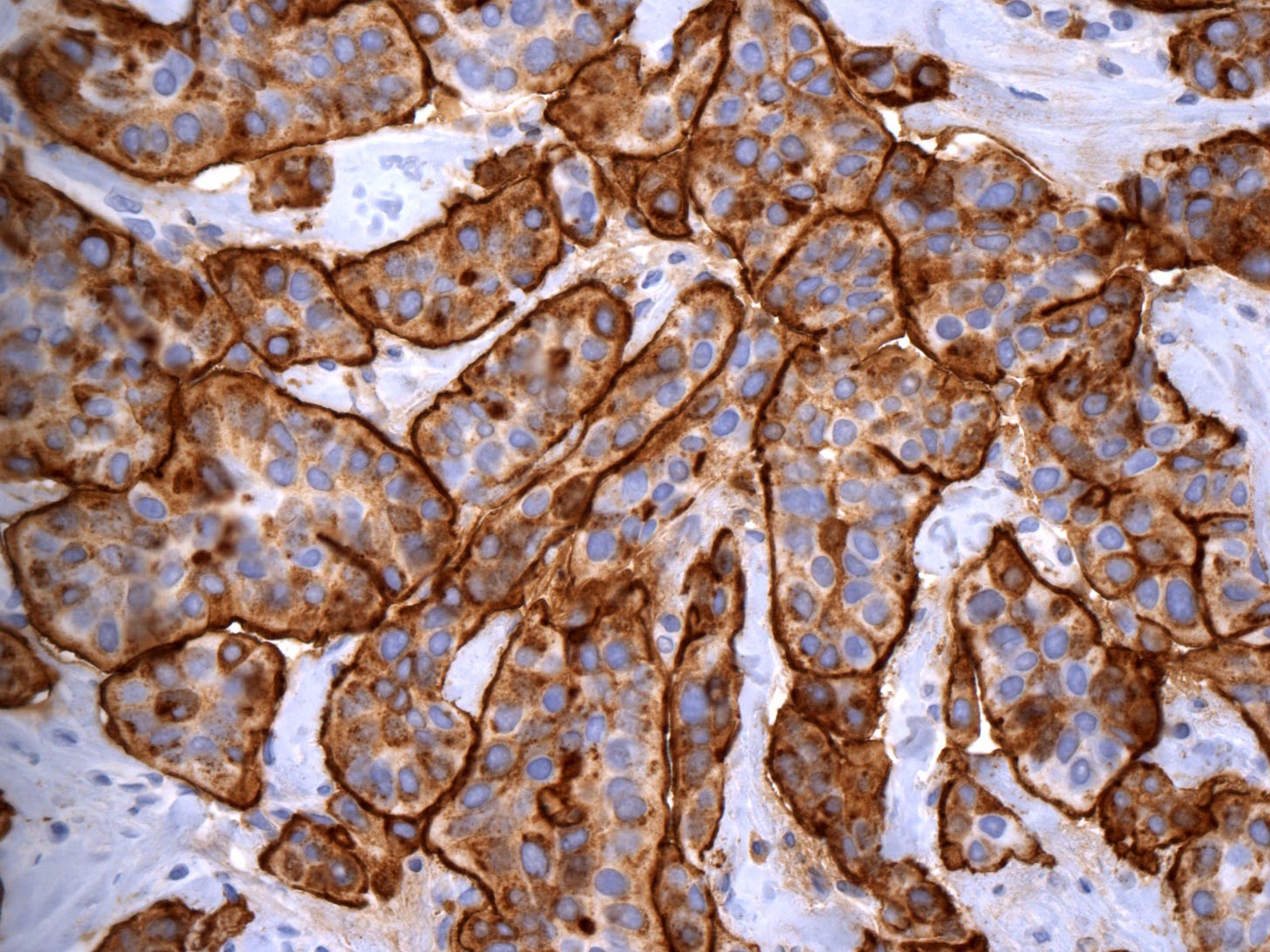
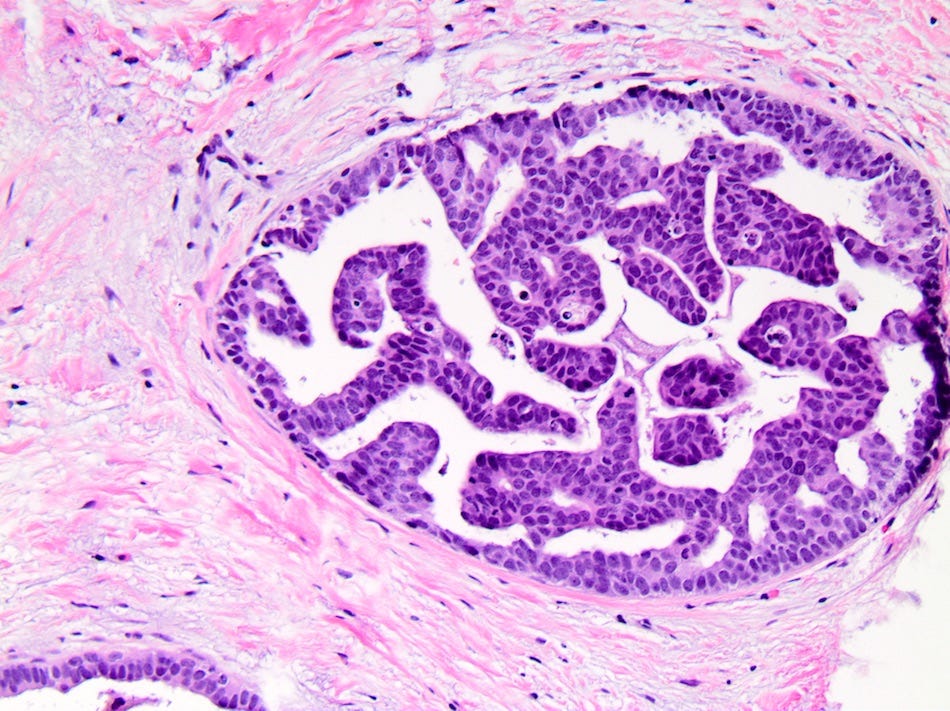
Invasive micropapillary carcinoma is an invasive breast cancer defined as having over 90% of the invasive component consisting of micropapillary carcinoma. It was first described in 1980 and given this name in 1993. It is characterized by pseudopapillary, tubular and morular epithelial structures with an “inside out” growth pattern, due to the reversal of the position of MUC1 (EMA) and other cell proteins (i.e., MUC1 is largely limited to the basal surface of the cells in contrast to conventional carcinomas in which MUC1 is largely apical, intracytoplasmic or intercellular).
In invasive micropapillary carcinoma, the micropapillae float in empty spaces and are often separated by delicate strands of fibrous stroma. It differs from papillary carcinoma because it has no fibrovascular cores. It has true angiolymphatic invasion in 78% of cases.
It represents only 2-7% of all breast cancers. It typically presents as a breast mass of 1.5 to 4 cm, often with positive lymph nodes and an advanced stage at presentation when compared with the usual type of breast carcinoma. Recent studies indicate it has a similar prognosis as the usual type of breast carcinoma, although prior studies reported a poorer prognosis. Effective treatment often requires extended surgical margins and vigilant preoperative axillary staging due to an increased incidence of lymph node invasion and locoregional recurrence. Tumors are typically ER positive and are eligible for antiestrogen treatment. Tumors are also associated with MUC4 immunohistochemistry expression, which may highlight the micropapillary component.
Invasive micropapillary carcinoma arises without an apparent precursor and has an unknown cause. It expresses a host of molecular changes indicative of the tumor cell’s ability to separate from neighboring cells and invade the vascular and lymphatic systems.
Micropapillary DCIS, which it resembles, is not considered a precursor. However, the presence of micropapillary DCIS is associated with poor prognostic factors: larger tumor size, higher tumor grade and nodal metastases.
Invasive micropapillary carcinoma may be associated with the upregulation of several nutrient transporters, which may contribute to the malignant potential by supporting the survival of cancer cells. This may resemble the hijacking of glycogen metabolism during the malignant transformation of glycogen rich carcinoma or the selection of the best metabolic program to sustain tumor progression by lipid rich carcinoma cells.
Micropapillary carcinoma - microscopic images
The next essay, part 6i, discusses mucin containing carcinomas of the breast without premalignant or preinvasive precursors and how they arise.
If you like these essays, please subscribe or share them with others.
Click here for the Index to Nat’s blog on Cancer and Medicine.
Follow me at https://www.linkedin.com/in/nat-pernick-8967765/ (LinkedIn), npernickmich (Threads and Instagram), natpernick.bsky.social (Bluesky) or @nat385440b (Tribel).
Follow our Curing Cancer Network through our Curing Cancer Newsletter, on LinkedIn or the CCN section of our PathologyOutlines.com blog. Each week we post interesting cancer related images of malignancies with diagnoses plus articles of interest. Please also read our CCN essays.
Latest versions of our cancer related documents:
American Code Against Cancer (how you can prevent cancer)
Email me at Nat@PathologyOutlines.com - Unfortunately, I cannot provide medical advice.
I also publish Notes at https://substack.com/note. Subscribers will automatically see my Notes.